Meningitis is a word that often strikes fear into the hearts of those who hear it. It’s a serious condition that can affect anyone, from infants to the elderly, and it requires immediate medical attention. But what exactly is meningitis? What causes it, and how is it treated? In this article, we’ll dive deep into the world of meningitis, breaking down the complex medical jargon into simple, easy-to-understand terms. By the end, you’ll have a clear understanding of this condition, its symptoms, causes, and the treatment options available.
What Is Meningitis?
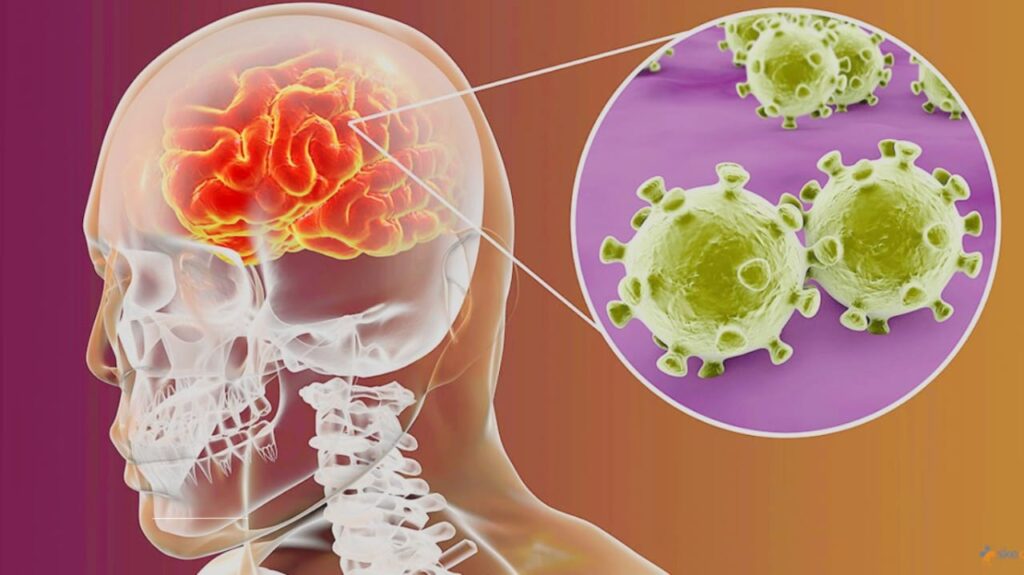
Meningitis is an inflammation of the meninges, the protective membranes that cover the brain and spinal cord. Think of the meninges as a thin, protective blanket that shields your central nervous system from harm. When these membranes become inflamed, it can lead to a range of symptoms, from mild headaches to life-threatening complications.
The inflammation is usually caused by an infection, but it can also result from non-infectious factors like certain medications, autoimmune diseases, or even physical injuries. Meningitis can be acute, developing rapidly over a few hours or days, or chronic, lasting for weeks or months.
Types of Meningitis
Meningitis isn’t a one-size-fits-all condition. There are several types, each with its own causes and characteristics. Understanding these types is crucial because the treatment and prognosis can vary significantly depending on the form of meningitis.
- Bacterial Meningitis
This is the most severe form of meningitis and requires immediate medical attention. It’s caused by bacteria such as Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. Bacterial meningitis can be life-threatening if not treated promptly, with a mortality rate of around 10-15%, even with treatment. - Viral Meningitis
Viral meningitis is the most common form and is generally less severe than bacterial meningitis. It’s often caused by enteroviruses, but other viruses like herpes simplex virus and mumps virus can also be responsible. Most people recover fully with supportive care, though the recovery process can take weeks. - Fungal Meningitis
This type is rare and usually occurs in individuals with weakened immune systems, such as those with HIV/AIDS or cancer. Fungi like Cryptococcus and Candida are common culprits. Fungal meningitis is treated with antifungal medications, but recovery can be slow. - Parasitic Meningitis
Parasitic meningitis is extremely rare and is caused by parasites like Naegleria fowleri, often referred to as the “brain-eating amoeba.” This form is almost always fatal, though cases are exceedingly uncommon. - Non-Infectious Meningitis
This type is caused by factors other than infections, such as certain medications, autoimmune diseases like lupus, or physical trauma. Treatment focuses on addressing the underlying cause.
Symptoms of Meningitis
The symptoms of meningitis can vary depending on the type and severity of the condition. However, there are some common signs to watch out for. These symptoms can develop suddenly or over a few days, and they often resemble those of the flu, which can make diagnosis challenging.
Common Symptoms in Adults and Older Children:
- Severe headache
- Stiff neck
- High fever
- Nausea and vomiting
- Sensitivity to light (photophobia)
- Confusion or difficulty concentrating
- Seizures
- Sleepiness or difficulty waking up
Symptoms in Infants and Young Children:
- High fever
- Constant crying
- Excessive sleepiness or irritability
- Poor feeding
- A bulge in the soft spot on the head (fontanelle)
- Stiffness in the body and neck
It’s important to note that not everyone with meningitis will experience all these symptoms. Some may only have a few, while others may exhibit more severe signs. If you or someone you know is experiencing symptoms that could indicate meningitis, seek medical attention immediately. Early diagnosis and treatment can make a significant difference in the outcome.
Causes and Risk Factors
Understanding the causes and risk factors of meningitis can help you take steps to reduce your risk. As mentioned earlier, the condition is often caused by infections, but other factors can also play a role.
Infectious Causes:
- Bacteria: Bacterial meningitis is typically spread through respiratory droplets or direct contact with an infected person. Outbreaks can occur in close quarters, such as college dormitories or military barracks.
- Viruses: Viral meningitis is often spread through fecal-oral contamination, respiratory droplets, or contact with an infected person’s saliva or mucus.
- Fungi: Fungal meningitis is usually contracted by inhaling fungal spores from the environment. It’s more common in individuals with compromised immune systems.
- Parasites: Parasitic meningitis is rare and is usually contracted through contaminated water.
Non-Infectious Causes:
- Medications: Certain drugs, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and antibiotics, can cause meningitis as a side effect.
- Autoimmune Diseases: Conditions like lupus or Behçet’s disease can trigger inflammation of the meninges.
- Physical Trauma: Head injuries or surgeries near the brain or spinal cord can lead to meningitis.
Risk Factors:
- Age: Infants, young children, and older adults are at higher risk.
- Weakened Immune System: People with HIV/AIDS, diabetes, or those undergoing chemotherapy are more susceptible.
- Living in Close Quarters: College students, military personnel, and people living in crowded conditions are at higher risk of bacterial meningitis.
- Travel: Visiting regions with high rates of certain infections, such as sub-Saharan Africa’s “meningitis belt,” can increase risk.
Diagnosis of Meningitis
Diagnosing meningitis involves a combination of clinical evaluation and diagnostic tests. If a healthcare provider suspects meningitis, they will typically perform the following:
- Physical Examination: The doctor will look for signs of infection, such as fever, and check for neck stiffness, which is a hallmark symptom of meningitis.
- Lumbar Puncture (Spinal Tap): This is the gold standard for diagnosing meningitis. A small amount of cerebrospinal fluid (CSF) is extracted from the lower back and analyzed for signs of infection or inflammation.
- Blood Tests: Blood samples may be taken to check for signs of infection, such as elevated white blood cell counts.
- Imaging Tests: In some cases, a CT scan or MRI may be performed to rule out other conditions or complications, such as brain swelling.
Treatment Options
The treatment for meningitis depends on the type and severity of the condition. Here’s a breakdown of the most common treatment approaches:
Bacterial Meningitis:
- Antibiotics: Immediate administration of intravenous antibiotics is crucial. The specific antibiotic used will depend on the type of bacteria causing the infection.
- Corticosteroids: These may be given to reduce inflammation and prevent complications like hearing loss.
- Supportive Care: This includes fluids, oxygen, and medications to manage symptoms like seizures or fever.
Viral Meningitis:
- Antiviral Medications: If the meningitis is caused by a virus like herpes simplex, antiviral drugs may be prescribed.
- Supportive Care: Most cases of viral meningitis resolve on their own with rest, hydration, and over-the-counter pain relievers.
Fungal Meningitis:
- Antifungal Medications: These are administered intravenously and may need to be continued for several weeks or months.
- Supportive Care: Similar to other types, this includes managing symptoms and ensuring the patient is comfortable.
Non-Infectious Meningitis:
- Addressing the Underlying Cause: If meningitis is caused by a medication, the drug will be discontinued. If it’s due to an autoimmune disease, immunosuppressive therapy may be used.
Prevention of Meningitis
Preventing meningitis involves a combination of vaccination, good hygiene practices, and awareness of risk factors.
Vaccination:
- Hib Vaccine: Protects against Haemophilus influenzae type b, a common cause of bacterial meningitis in children.
- Pneumococcal Vaccine: Protects against Streptococcus pneumoniae.
- Meningococcal Vaccine: Protects against Neisseria meningitidis.
- MMR Vaccine: Protects against measles, mumps, and rubella, which can lead to viral meningitis.
Hygiene Practices:
- Wash your hands frequently, especially before eating or touching your face.
- Avoid sharing utensils, drinks, or personal items with others.
- Practice safe food and water hygiene, particularly when traveling.
Awareness:
- Be aware of the symptoms of meningitis and seek medical attention promptly if they occur.
- If you’re at higher risk due to travel or living conditions, talk to your healthcare provider about preventive measures.
