Understanding the Hidden Toll on Your Kidneys
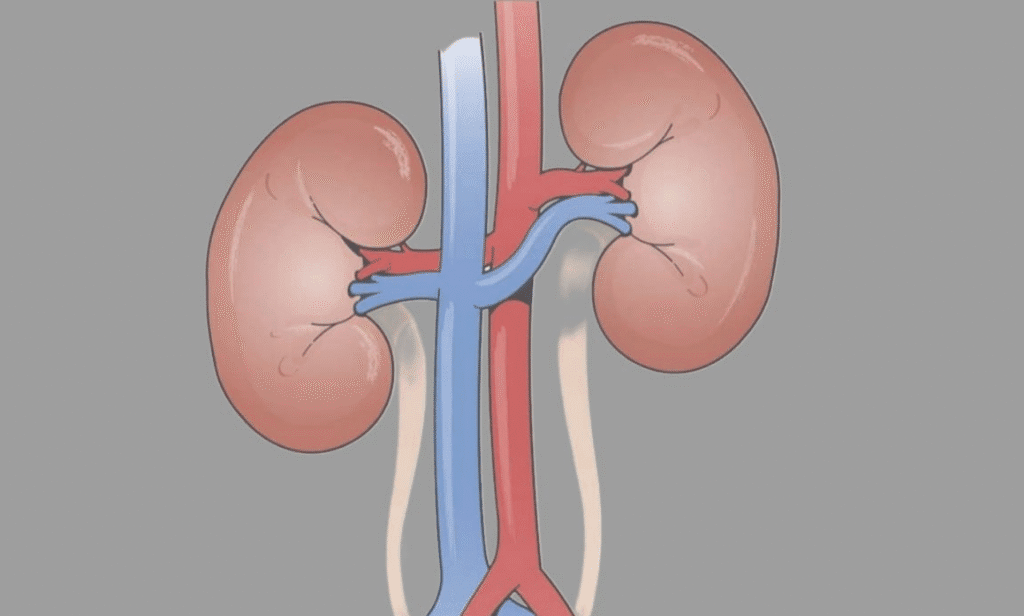
Your kidneys might be small—about the size of your fist—but they pull off a Herculean task every day. These bean-shaped organs filter around 200 liters of blood, flushing out waste and balancing fluids to keep your body humming along. When things go wrong, though, the fallout can be serious: from painful kidney stones to chronic kidney disease (CKD), which affects over 37 million adults in the U.S. alone, according to the National Kidney Foundation. Diet plays a starring role here, and surprisingly, some of our go-to foods can turn into silent saboteurs if we overdo it. As a nephrologist with over 15 years in the field, I’ve seen patients blindsided by their plates—folks who thought a salty snack or a steak dinner was harmless until lab tests showed creeping creatinine levels. The good news? Awareness is your first line of defense. Let’s dive into seven common culprits, breaking down why they strain the kidneys and how to enjoy life without the regret.
Kidneys thrive on balance, but modern eating habits often tip the scales. High-sodium meals force these filters to retain water, spiking blood pressure that batters delicate vessels over time. A study in the Journal of the American Society of Nephrology found that just one extra gram of sodium daily ups CKD risk by 17%. It’s not about swearing off favorites entirely; it’s about mindful portions. Think of your kidneys as overworked baristas—too many demanding orders, and the espresso machine (your renal function) starts sputtering. By spotting these foods, you empower yourself to tweak habits that safeguard long-term vitality.
Salt: The Sneaky Seasoner That Overloads Renal Workload
Salt—sodium chloride in its simplest form—has earned its villain status in kidney conversations for good reason. Every pinch you sprinkle or slurp from a soup can seems innocent, but excess sodium signals your kidneys to hold onto water like a sponge. This fluid buildup raises blood pressure, and chronic hypertension is the leading cause of kidney damage, per the Centers for Disease Control and Prevention (CDC). Imagine your kidneys as tiny pumps; too much salt clogs the pipes, making them labor overtime to excrete the surplus.
In my clinic, I’ve treated countless patients whose love for fast-casual eats masked a sodium bomb. One middle-aged accountant, let’s call him Raj, came in with swelling in his ankles after years of daily deli sandwiches. His blood pressure hovered at 150/95, and early glomerular filtration rate (GFR) tests flagged mild impairment. Cutting sodium to under 2,300 milligrams daily—ideally 1,500 for those at risk—turned things around in months. Processed items like canned beans or frozen pizzas pack 1,000 milligrams per serving, dwarfing the quarter-teaspoon of table salt.
Why does this hit kidneys so hard? Sodium disrupts the renin-angiotensin system, a hormonal cascade that regulates blood flow. Over time, it leads to glomerulosclerosis—scarring of the filtering units—reducing efficiency by up to 20% in heavy consumers, as noted in a Lancet study. For folks with diabetes or existing CKD, the stakes skyrocket; the American Heart Association links high-salt diets to a 28% higher end-stage renal disease risk. But here’s the silver lining: fresh herbs like rosemary or citrus zests swap in seamlessly, flavoring without the fallout. Track your intake with apps like MyFitnessPal, and watch how small swaps ease the renal strain.
Beyond direct damage, salt exacerbates other issues. It promotes calcium excretion in urine, a precursor to stones—those excruciating crystals that sideline 1 in 10 Americans yearly. A Harvard cohort study of 81,000 women revealed that the saltiest eaters faced 30% more stone episodes. So, next time you reach for chips, pause: is that crunch worth the hidden hassle for your kidneys?
Red Meat: Protein Powerhouse or Purine Peril?
Red meat—think juicy steaks, burgers, or lamb chops—delivers a protein punch that’s muscle-building gold for athletes and everyday folks alike. But when it dominates your plate, the kidneys pay a steep price. Loaded with purines, these compounds break down into uric acid, which, in excess, crystallizes into stones or triggers gouty flares that inflame renal tissues. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) reports that high-purine diets correlate with a 40% uptick in uric acid kidney stones.
From my experience, weekend grill masters often underestimate the toll. Take Maria, a 45-year-old teacher who indulged in red meat thrice weekly. Her annual checkup uncovered elevated uric acid at 7.5 mg/dL—above the 6.0 threshold—and microalbuminuria signaling early damage. We dialed back to leaner cuts twice a week, folding in plant proteins like lentils, and her levels normalized. Science backs this: a meta-analysis in the American Journal of Clinical Nutrition showed that swapping 3 ounces of beef for fish or tofu slashes uric acid by 12%.
The strain isn’t just from purines; red meat’s saturated fats hike cholesterol, fostering plaque in renal arteries. This atherosclerosis narrows blood flow, starving nephrons of oxygen and hastening atrophy. For those with CKD stages 3-5, the Kidney Disease Outcomes Quality Initiative recommends capping animal protein at 0.8 grams per kilogram of body weight daily to preserve residual function. Overindulgence? It can accelerate progression by 2-3 times, per European Renal Association data.
Yet, red meat’s appeal endures—its heme iron absorbs effortlessly, warding off anemia. Balance is key: pair it with veggies rich in potassium, like spinach, which counters acid load. A DASH diet trial involving 4,000 participants demonstrated that moderated red meat intake, alongside fruits, dropped CKD markers by 15%. Grill smarter, not harder, and your kidneys will thank you with steadier performance.
Processed Foods: Convenience Traps Packed with Renal Toxins
Ah, processed foods—the unsung heroes of busy lives, from microwave burritos to boxed mac ‘n’ cheese. They promise speed, but at what cost to your kidneys? These shelf-stable stars brim with sodium (up to 80% of daily intake from them, says the FDA), phosphates for preservation, and artificial additives that baffle renal detox pathways. A single frozen dinner can clock 1,500 milligrams of sodium, forcing kidneys into hyperdrive and elevating pressure that erodes filtration over years.
I’ve counseled families where “easy weeknights” masked a renal reckoning. One patient, a software engineer named Liam, scarfed convenience meals amid deadlines. His eGFR dipped to 75 mL/min, and urine tests showed proteinuria. Auditing his pantry revealed 3,000+ milligrams sodium daily—double the guideline. Swapping to home-prepped stir-fries with whole grains reversed the slide, restoring baseline in six months. Research from the Framingham Heart Study echoes this: processed-heavy diets boost CKD odds by 25%.
Phosphates deserve a spotlight too. Added to sodas and snacks for tang, they bind calcium, forming deposits in kidneys—think vascular calcification that stiffens arteries. The Journal of Renal Nutrition links high-phosphate processed intake to a 22% faster CKD decline. Additives like MSG or nitrates? They inflame gut linings, indirectly taxing kidneys via toxin spillover.
For credibility, consider Dr. Sharon Moe, a Purdue nephrologist whose trials show phosphate binders cut absorption by 50% in at-risk groups. But prevention trumps cure: read labels (aim under 5% daily value per serving) and batch-cook staples like quinoa salads. A UK Biobank analysis of 500,000 adults found whole-food eaters had 18% lower renal disease rates. Convenience doesn’t have to compromise; it’s about choosing allies, not adversaries, for your kidneys.
Sugary Drinks: Sweet Sips That Fuel Renal Fire
Sugary drinks—colas, energy shots, fruit punches—quench thirst with a sugar rush, but they douse your kidneys in trouble. High-fructose corn syrup spikes blood glucose, fostering insulin resistance that thickens glomerular basement membranes, per a Diabetes Care review. Worse, phosphoric acid in dark sodas leaches calcium from bones, concentrating it in urine for stone formation. The Nurses’ Health Study tracked 90,000 women, finding daily soda drinkers 33% more prone to stones.
In practice, I’ve seen young professionals hit hard. Sarah, a 32-year-old marketer, downed two cans daily for “pick-me-ups.” Her HbA1c crept to 6.2, and a CT scan revealed a 5mm stone. We replaced with infused water—lemon and mint—and her urinary pH balanced, dissolving risks. Stats from the CDC: sugary beverage fans face 26% higher CKD incidence, tied to obesity’s renal burden.
Phosphorus additives amplify the issue, suppressing parathyroid hormone and disrupting mineral balance. A Clinical Journal of the American Society of Nephrology study on 3,000 adults showed top-quartile consumers had 1.5 times the progression risk. Dehydration compounds it; caffeine-laced versions act as diuretics, concentrating waste.
Expert insight from Dr. Kalantar-Zadeh, UC Irvine’s CKD guru, highlights zero-sugar swaps like sparkling water with berries, cutting exposure by 90%. A Mediterranean-style trial in The Lancet reduced sugary intake, yielding 20% better eGFR after a year. Sip wisely—your kidneys crave hydration, not hidden havoc.
Dairy Products: Creamy Comforts Crossing Calcium Lines
Dairy—milk, cheese, yogurt—nurtures bones with calcium and vitamin D, but excess tips into kidney trouble. High intake floods the system with phosphorus and animal proteins, acidifying urine and promoting stones. The Oxford EPIC cohort of 8,000 men linked daily high-dairy diets to 62% more calcium oxalate stones.
Patients like Tom, a 50-year-old retiree loving his cheddar, illustrate the pivot point. Weekly cheese boards masked phosphorus overload; his serum levels hit 4.8 mg/dL, straining filtration. Moderating to low-fat options and plant milks dropped it to 3.5. The International Osteoporosis Foundation notes dairy’s acid load burdens kidneys, accelerating decline in stage 2 CKD by 15%.
Calcium paradox: while protective in moderation, surplus binds oxalates but overwhelms excretion. A JAMA Internal Medicine analysis of 4,500 adults found over-1,200mg daily calcium from dairy hiked stone risk 20%. For lactose-intolerant or vegan crowds, fortified almond milk sidesteps this.
Renal dietitian Elena Ramirez advises portioning: one serving per meal. A DASH-sodium trial incorporating controlled dairy improved renal outcomes by 12%. Indulge thoughtfully—dairy’s perks shine without the excess edge.
Caffeine: The Buzz That Drains Kidney Reserves
Caffeine, that morning jolt from coffee or tea, sharpens focus but saps kidney hydration. As a mild diuretic, it boosts urine output, concentrating minerals that crystallize into stones. The American Journal of Epidemiology reports daily 300mg+ (three coffees) users face 10% higher stone odds.
I’ve guided baristas-turned-patients through this. Alex, a 28-year-old barista, chugged four espressos daily; dehydration showed in BUN/creatinine ratios, and ultrasound caught crystals. Capping at 200mg with electrolyte waters cleared it. Harvard’s Health Professionals Follow-up Study ties high caffeine to 23% elevated CKD risk via pressure spikes.
Adenosine blockade ramps heart rate, stressing vessels. Chronic? It fosters interstitial nephritis. Dr. Sophie Lederman, a caffeine researcher, notes tolerance varies—genetics play in via CYP1A2 enzyme. Balance with decaf or green tea’s antioxidants, which a Nutrients study showed protect against oxidative renal stress.
A 10-year Taiwanese cohort found moderate (under 200mg) intake neutral, but excess accelerated GFR loss by 8%. Brew mindfully—caffeine’s spark needn’t dim your kidneys’ glow.
Fried and Fast Foods: Crispy Cravings Clogging Renal Pathways
Fried and fast foods—fries, nuggets, drive-thru delights—tempt with crunch, but their trans fats, sodium, and acrylamides choke kidney flow. High-heat frying births advanced glycation end-products (AGEs) that inflame nephrons, per a Kidney International review. The CDC flags fast-food regulars for 21% higher obesity-linked CKD.
One patient, Javier, a 40-year-old trucker, lived on fries; his BMI hit 32, and albuminuria emerged. Swapping air-fried veggies trimmed waist and stabilized function. A Framingham Offspring Study links weekly fast-food binges to 30% vascular damage risk.
Sodium and fats synergize: hypertension plus atherosclerosis halves renal blood flow. Dr. Lyn Steffen, University of Minnesota epidemiologist, cites trials where cutting fried intake boosted eGFR 10%. Opt for oven-baked—flavor without the fry.
A global INTERHEART analysis of 15,000 cases showed fried-heavy diets up chronic disease by 25%, kidneys included. Savor sparingly; your renal engines deserve cleaner fuel.
