When we talk about human papillomavirus (HPV), most people think of cervical cancer and women’s health. But here’s the truth: HPV doesn’t discriminate. Men are equally at risk of infection—and the consequences can be life-altering. From genital warts to cancers of the throat, penis, and anus, HPV poses silent threats that often fly under the radar. Let’s break down what every man (and those who care about them) needs to know.
HPV 101: The Virus You’ve Probably Already Encountered
HPV is the most common sexually transmitted infection globally. Of its 200+ strains, about 40 affect the genital area. While most infections clear on their own, certain “high-risk” strains (like HPV 16 and 18) can linger, causing cell changes that lead to cancer. Others cause benign but bothersome issues like genital warts.
Key Stats:
- 80% of sexually active people get HPV at some point.
- 50% of infections occur in adults aged 15–25.
- 1 in 4 men in the U.S. have a high-risk oral HPV strain.
How Do Men Get HPV?
HPV spreads through skin-to-skin contact, not just bodily fluids. This means condoms reduce but don’t eliminate risk. Common transmission routes include:
- Vaginal, anal, or oral sex
- Intimate touching (e.g., genital contact without penetration)
- Shared sex toys
“HPV is stealthy. You don’t need symptoms to spread it,” says Dr. Marcus Lin, a urologist specializing in men’s sexual health. “Many men carry the virus unknowingly for years.”
Health Risks for Men: More Than Just Warts
1. Cancers Linked to HPV
While cervical cancer gets the spotlight, HPV causes 70% of oropharyngeal (throat) cancers in men—a rate that’s tripled since the 1980s. It’s also responsible for:
- 90% of anal cancers
- 60% of penile cancers
Case in Point: Michael Douglas made headlines in 2013 when he revealed his throat cancer was linked to HPV. His story shifted public awareness, but many still underestimate the risk.
2. Genital Warts
Low-risk HPV strains (6 and 11) cause 90% of genital warts. While non-cancerous, they can recur, require treatment, and impact mental health.
3. Fertility Concerns
Emerging research suggests HPV may reduce sperm quality, though more studies are needed.
Why Men Often Fly Under the Radar
- No Routine Screening: Unlike cervical Pap smears for women, there’s no approved HPV test for men.
- Delayed Symptoms: Throat cancers, for example, often surface decades after infection.
- Stigma: Men are less likely to report symptoms or seek care for sexual health issues.
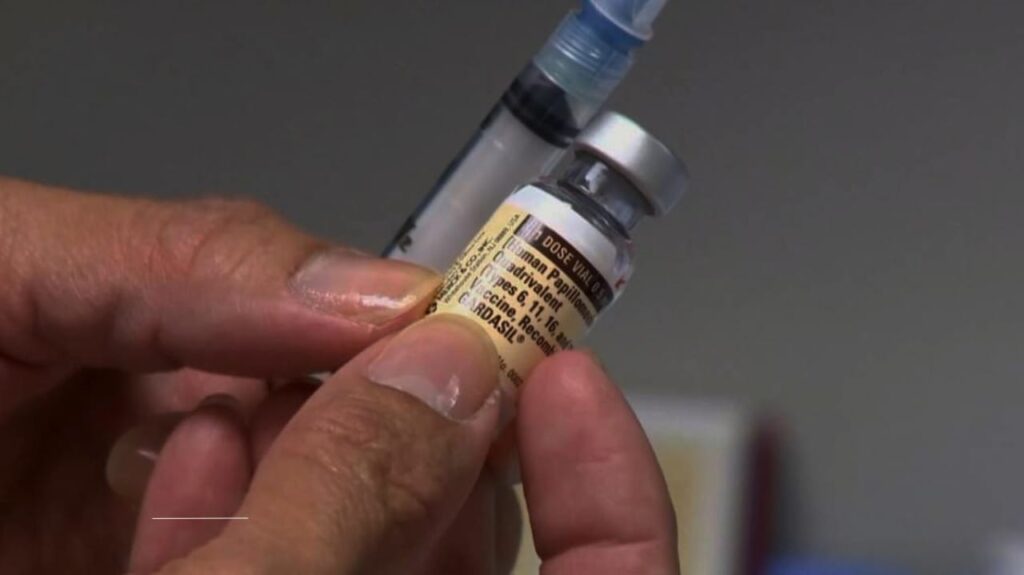
The HPV Vaccine: Not Just for Teen Girls
The HPV vaccine (Gardasil 9) protects against 9 high-risk strains. Initially marketed for girls, it’s now recommended for boys and men up to age 45. Yet, vaccination rates lag:
- 72% of girls aged 13–17 in the U.S. are vaccinated vs. 62% of boys.
- In Canada, less than 40% of eligible males have received the vaccine.
Myth Buster: “The vaccine isn’t just for teens,” emphasizes Dr. Sarah Jennings, an infectious disease specialist. “Even if you’re sexually active, it can protect against strains you haven’t encountered.”
Prevention Beyond the Shot
- Safe Sex Practices: Condoms and dental dams reduce (but don’t eliminate) transmission.
- Regular Check-Ups: Report unusual lumps, sores, or persistent throat pain to your doctor.
- Anal Pap Smears (For High-Risk Groups): Recommended for gay, bisexual, and immunocompromised men.
Breaking the Silence: Men’s Health and HPV
Cultural stereotypes about masculinity often keep men from discussing sexual health. “I’ve had patients dismiss symptoms for years because they feared judgment,” shares Dr. Lin. Open conversations with partners and healthcare providers are critical.
The Bigger Picture: Global Disparities
In low-income countries, limited vaccine access and stigma amplify risks. For example:
- 85% of HPV-related cancers occur in developing nations.
- Only 20% of African nations include boys in HPV vaccination programs.
What the Future Holds
Researchers are exploring therapeutic vaccines for existing infections and better screening tools. Meanwhile, advocacy groups push for gender-neutral vaccination policies.
Final Note to Readers:
HPV is a shared responsibility. Whether you’re a parent considering vaccination for your son, a partner encouraging a check-up, or a man rethinking your own health habits, knowledge is power. Stay informed, stay proactive, and remember: prevention is always better than cure.
