Florida Faces an Early and Active Flu Season, Health Officials Urge Vaccination
Health authorities across Florida are signaling a clear message to residents: the influenza virus is circulating earlier and more aggressively than in recent years. A noticeable uptick in confirmed flu cases and related hospitalizations is prompting a strong push from medical professionals for the public to take proactive steps. The current data suggests a flu season that could peak sooner than the typical winter surge, making immediate action crucial for community-wide protection. This trend isn’t isolated to Florida; several southern states are reporting similar patterns, indicating a regional viral spread. Understanding the dynamics of this early season is the first step in building an effective defense for you and your family.
Current Data on Influenza Activity in the State
Recent reports from the Florida Department of Health paint a concerning picture of viral activity. Surveillance systems are tracking a steady increase in positive influenza tests from outpatient clinics, emergency departments, and hospital networks. While specific numbers fluctuate weekly, the trajectory shows a consistent climb, with certain regions, including parts of South Florida and the Tampa Bay area, experiencing higher concentrations of cases. Hospitalizations, particularly among adults over the65 and very young children, have begun to rise, putting a strain on healthcare facilities. This data is not meant to cause alarm but to provide a factual basis for the recommendations that follow, empowering residents with knowledge.
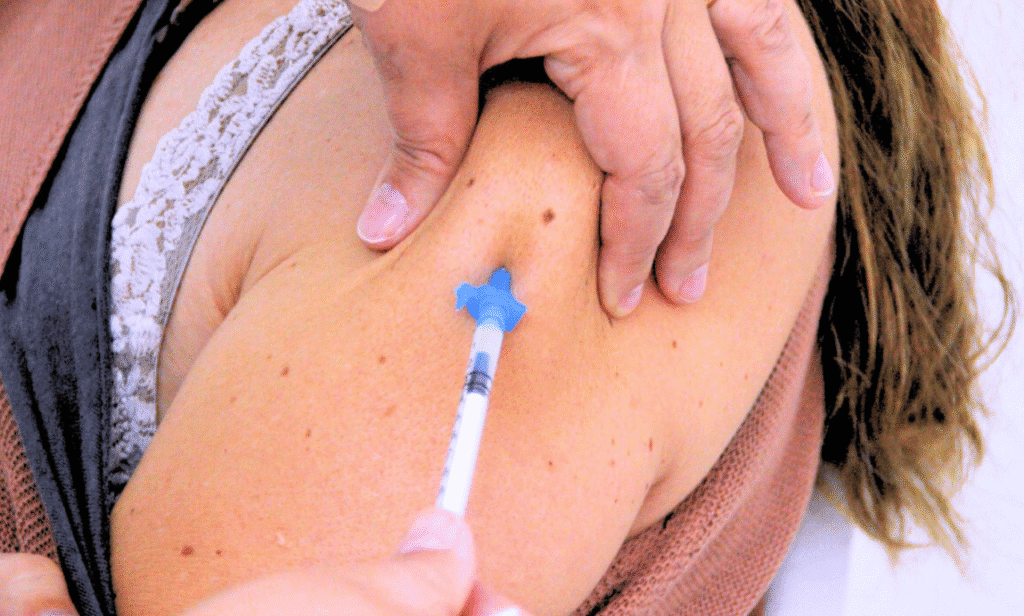
Why Vaccination Remains Your Strongest Defense Against the Flu
The single most effective tool for preventing severe illness, hospitalization, and death from influenza is the annual flu shot. The vaccine works by prompting your immune system to produce antibodies that fight the virus. It takes roughly two weeks for these antibodies to develop fully, which is why getting vaccinated now is critically important. Dr. Elena Rodriguez, an infectious disease specialist based in Miami, explains, “The flu vaccine is not a forcefield; it’s training for your immune system. Even if you contract a strain not perfectly matched by the vaccine, that ‘training’ often means your body fights the virus more effectively, leading to a much milder and shorter illness.” This reduces the risk of severe complications like pneumonia.
Identifying the Most Vulnerable Populations During Flu Season
While influenza can seriously affect anyone, specific groups face a significantly higher risk of developing dangerous complications. These vulnerable populations include adults aged 65 and older, whose immune systems may have a weaker response to infection. Young children, especially those under 5, are also at high risk because their immune systems are still developing. Other groups include pregnant women, individuals with chronic health conditions like asthma, heart disease, or diabetes, and those with compromised immune systems. For people in these categories, what might be a week of misery for a healthy adult can quickly escalate into a life-threatening situation requiring intensive medical care.
Beyond the Shot: Everyday Habits to Reduce Your Risk of Illness
Vaccination is the cornerstone of flu prevention, but it should be part of a broader strategy of healthy habits. Consistent and thorough handwashing with soap and water for at least 20 seconds is one of the simplest and most powerful ways to remove germs. If soap isn’t available, an alcohol-based hand sanitizer is a good alternative. Make a conscious effort to avoid touching your eyes, nose, and mouth with unwashed hands, as these are primary entry points for the virus. Regularly cleaning and disinfecting frequently touched surfaces at home and work, such as doorknobs, light switches, and countertops, can also help break the chain of transmission.
The Critical Importance of Staying Home When You Feel Unwell
One of the most socially responsible actions you can take during flu season is to stay home from work, school, and public gatherings when you are sick. The influenza virus is highly contagious and can spread through droplets when an infected person coughs, sneezes, or even talks. By isolating yourself, you create a barrier that protects your colleagues, classmates, and the broader community. This is especially vital in settings with high-risk individuals. Pushing through illness is not a badge of honor; it contributes to the wider spread of the virus and prolongs the season for everyone.
How Widespread Vaccination Contributes to Community Immunity
The concept of ‘herd immunity’ or community immunity is a powerful public health benefit of vaccination. When a sufficiently high percentage of a community is immunized against a contagious disease, it becomes difficult for the virus to find new hosts and spread. This creates a protective buffer that helps shield those who cannot be vaccinated, such as newborns or individuals with certain severe allergies, or those for whom the vaccine is less effective, like the immunocompromised. High vaccination rates in a community can effectively slow or even stop outbreaks, protecting the most fragile among us.
Recognizing the Symptoms: When to Seek Medical Attention
Distinguishing between the common cold and influenza is important for determining the right course of action. Flu symptoms often come on abruptly and typically include fever, chills, muscle aches, fatigue, headache, and a dry cough. A runny nose and sore throat are more common with a cold. Most healthy adults can manage flu symptoms at home with rest, fluids, and over-the-counter fever reducers. However, it is essential to seek medical care if you or a family member experiences difficulty breathing, persistent chest pain, sudden dizziness, confusion, severe vomiting, or if flu symptoms improve but then return with a worse fever and cough.
The Strain on Florida’s Healthcare System During Peak Flu Season
Hospitals and clinics throughout Florida are preparing for the annual influx of patients that accompanies the peak of flu season. Increased hospitalizations for influenza and related complications like pneumonia can place a significant burden on emergency departments, inpatient beds, and healthcare staff. This surge can lead to longer wait times and can strain resources, potentially impacting the care available for other medical emergencies. By taking preventive measures like getting vaccinated, the public can play a direct role in reducing this burden, ensuring that medical services remain available for those who need them most.
Addressing Common Myths and Misconceptions About the Flu Vaccine
Despite decades of evidence supporting its safety and efficacy, misinformation about the flu vaccine persists. A common myth is that the flu shot can give you the flu. This is scientifically impossible, as the injectable vaccine is made with either an inactivated (killed) virus or a single gene from the virus, not the whole, live virus. Another misconception is that healthy people don’t need the vaccine. Even healthy individuals can become severely ill from the flu, and they can also unknowingly transmit the virus to more vulnerable friends, family, or colleagues. The vaccine is a protective measure for both the individual and the community.
