The landscape of organ transplantation is undergoing a seismic shift, moving from the realm of science fiction into tangible clinical reality. In a landmark achievement that promises to redefine the future of medicine, surgeons have successfully transplanted a genetically modified pig liver into a living human patient. This procedure, a world-first, was not a permanent organ replacement but a critical, life-sustaining bridge. The patient, suffering from acute liver failure and too ill for a conventional human liver transplant, was connected to the pig liver outside their body. For three days, the animal organ functioned flawlessly, filtering toxins and producing vital proteins, keeping the patient stable and conscious until a suitable human liver became available. This extraordinary success represents the most significant advance to date in the field of xenotransplantation—the process of using animal organs in humans—and offers a powerful beacon of hope for the tens of thousands of patients on transplant waiting lists.
This breakthrough did not happen overnight. It is the culmination of decades of painstaking research, failure, and incremental progress. The fundamental challenge with using animal organs is the human immune system’s violent and immediate rejection of foreign tissue. Early attempts at cross-species transplants faltered because the body would recognize the organ as an invader and mount a devastating attack. The key to overcoming this has been genetic engineering. The pig used in this historic procedure was not from a standard farm. It was bred by a specialized company, Revivicor, a subsidiary of United Therapeutics, and was genetically altered with a remarkable level of precision. Scientists removed specific pig genes that produce sugars on the surface of cells, sugars that the human immune system instantly recognizes as a threat. Furthermore, they inserted several human genes that produce proteins responsible for regulating immune responses, blood clotting, and other critical functions. This genetic “humanization” of the pig organ was essential to trick the recipient’s body into accepting the temporary biological assistant.
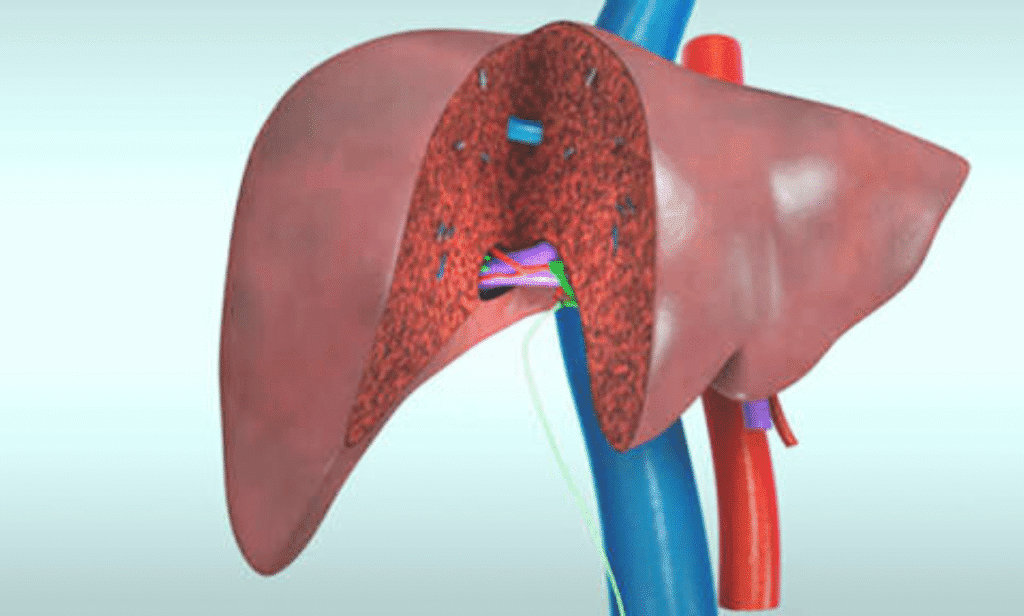
The patient, a man in his fifties, was facing almost certain death. His liver had failed catastrophically, a condition with a mortality rate exceeding 80% without a transplant. He was experiencing hepatic encephalopathy, a brain disorder caused by the liver’s inability to remove toxins from the blood, and was slipping into a coma. With no human liver available and his condition deteriorating by the hour, the medical team at a leading academic hospital, in collaboration with an extensive ethics board and regulatory bodies, made the decision to pursue the experimental pig liver support. The procedure, known as extracorporeal perfusion, is technically distinct from a full transplant. The pig liver was housed in a device outside the patient’s body. The patient’s blood was carefully circulated through this device, allowing the pig liver to perform the essential duties of a human liver without being physically implanted. This method significantly reduces the immediate risks of rejection and infection compared to a full internal transplant.
The results were nothing short of spectacular. Within hours of the connection, the patient’s clinical status began to stabilize. Key biomarkers told a compelling story. Levels of ammonia, a potent neurotoxin that the liver is supposed to clear, plummeted. The patient’s bilirubin, a yellow pigment that builds up during liver failure, causing jaundice, also showed a significant decrease. Most importantly, the pig liver began producing albumin, a crucial protein made by the liver that maintains blood volume and carries substances through the bloodstream. The patient’s own albumin levels started to rise. Clinically, the most dramatic change was in his mental status. The man, who had been comatose and on a ventilator, began to wake up. He regained consciousness, was able to follow commands, and was eventually taken off the ventilator while the pig liver was still supporting his system. This neurological improvement provided the most visceral evidence that the procedure was working.
This medical triumph is part of a broader wave of innovation in xenotransplantation. In recent years, the field has witnessed several critical milestones that have built upon one another. The first successful transplantation of a genetically modified pig heart into a living human, performed at the University of Maryland Medical Center in 2022, paved the way for this latest achievement. While that patient lived for two months, the procedure proved that such cross-species organ replacements could function in the human body for a meaningful period. More recently, surgeons at NYU Langone Health and the University of Pennsylvania have conducted temporary pig kidney transplants into brain-dead donors, with the organs functioning for record-breaking periods, in one case for over two months. These experiments in deceased recipients provided invaluable safety and efficacy data, demonstrating that the organs could filter blood and produce urine without being hyper-acutely rejected. The successful pig liver procedure in a living patient is the next logical, yet profoundly significant, step in this sequential clinical journey.
The implications of this success are monumental for the field of transplant medicine. The primary driver for this research is the dire and unrelenting organ shortage. In the United States alone, over 100,000 people are on the national transplant waiting list, and tragically, an average of 17 people die each day waiting for an organ. The liver is the second most needed organ after the kidneys. The ability to use readily available, genetically engineered pig organs as a bridge to transplant, or potentially as a permanent solution in the future, could effectively eliminate waiting list mortality. It would transform organ transplantation from an emergency procedure reliant on tragic events into a scheduled, planned surgery. This shift would not only save countless lives but also dramatically improve patient outcomes, as individuals could receive transplants before they become critically ill and debilitated by their organ failure.
Despite the euphoria surrounding this achievement, the medical team and the broader scientific community are proceeding with cautious optimism. A three-day success is a powerful proof of concept, but it raises a host of new questions that only further research can answer. The long-term viability of pig organs in humans remains the ultimate unknown. Could a pig liver function for years, or even decades, inside a human body? Researchers are closely monitoring two major long-term risks beyond initial rejection. The first is the potential for zoonosis, the transmission of animal viruses to humans. While the donor pigs are raised in meticulously sterile, closed environments to prevent infections, the theoretical risk of an unknown porcine endogenous retrovirus (PERV) activating in a human host is a top concern for regulatory agencies like the FDA. The second major challenge is physiological compatibility. While the pig liver performed key functions perfectly, subtle differences in its protein production or metabolic processes could have unforeseen long-term effects on a human recipient.
The ethical dimensions of breeding animals for organ harvesting are complex and demand serious public discourse. Proponents argue that the potential to save tens of thousands of human lives justifies the use of animals, particularly when those animals are treated humanely in controlled environments. They point to the widespread consumption of pigs for food as a contextual factor. However, bioethicists raise important questions about the moral status of genetically altered animals and the “instrumentalization” of life. Informed consent from patients and their families in these desperate, life-or-death situations is another critical area of focus. The teams involved in these trials work with dedicated ethics boards to ensure that patients fully understand the experimental nature of the procedure and the potential unknown risks. Public trust, built on transparency and rigorous oversight, will be essential for xenotransplantation to gain widespread acceptance.
The financial and logistical aspects of creating a supply of transplant-ready pig organs are staggering. The genetic engineering, cloning, and breeding of these animals in ultra-clean, pathogen-free facilities is an incredibly expensive endeavor, costing tens of millions of dollars in research and development. If this technology is to become a mainstream medical therapy, a scalable and economically viable model must be developed. This will require significant investment, partnerships between biotech firms and hospital systems, and eventually, discussions with health insurance providers about coverage. The goal is to make xenotransplantation not just a scientific curiosity, but an accessible and cost-effective treatment for the masses, preventing the technology from becoming a luxury available only to the wealthy.
The patient at the center of this medical drama is now recovering after receiving his human liver transplant. His story is a testament to human resilience and scientific ingenuity. He served as the first living proof that a genetically engineered animal organ can successfully and safely sustain human life. His case provides a treasure trove of data that will be analyzed for years to come. Researchers are studying his immune response, the detailed function of the pig liver, and the physiological interactions between man and animal organs. Every piece of data brings science closer to the next milestone. The success of this procedure has already energized the field, with plans for more rigorous clinical trials involving small groups of patients. These future studies will aim to extend the duration of support, refine the anti-rejection drug regimens, and further assess the safety profile. The path forward is one of careful, deliberate steps, but the direction is clear. A new source of organs is no longer a distant dream but an emerging reality, offering a future where no one has to die waiting for a transplant.
