New research delivers a powerful and urgent message to women approaching their fifth decade: attending that very first breast cancer screening invitation at age 40 is not just a routine check-up; it could be a decisive factor in your long-term survival. A significant study, shaking up conventional conversations around preventative care, has found that women who skip their initial mammogram at 40 face a substantially higher risk of dying from breast cancer later in life. This isn’t about a slight statistical bump. The findings point to a dramatic increase in risk, turning what might have been a low-priority appointment into a potentially life-saving obligation. The implications are profound, suggesting that the first screening acts as a critical baseline, a foundational moment for detecting aggressive, fast-moving cancers that can emerge in a woman’s 40s. For years, the debate has often centered on the frequency of screenings or the ideal starting age. This new evidence shifts the focus squarely onto the importance of that initial encounter with the healthcare system, highlighting it as a pivotal point of intervention.
The study, which analyzed data from a large population of women over many years, aimed to understand the long-term outcomes based on participation in the very first screening round. Traditionally, the effectiveness of screening programs is measured by comparing screened versus unscreened populations over time. This research took a more nuanced approach, isolating the impact of that first crucial test. What they discovered was striking. Women who did not attend their first scheduled screening at age 40 showed a significantly higher rate of late-stage breast cancer diagnoses in the subsequent years. The key issue is the stage at which cancer is detected. Cancers found early, often when they are small and haven’t spread, are highly treatable, with five-year survival rates exceeding 90%. Cancers diagnosed at a later stage, after symptoms have appeared, are far more challenging to treat successfully. The study suggests that missing that first screening creates a dangerous gap, allowing cancers that develop in the early 40s to progress undetected until they become more advanced and deadly.
So, why is this first screening at 40 so uniquely important? Experts explain that the breast tissue of women in their 40s is typically denser than in older women. Dense breast tissue can make mammograms harder to read, as both tumors and dense tissue appear white on the image. This is precisely why some have questioned the efficacy of screening in this age group. However, this new research turns that argument on its head. It posits that establishing a baseline mammogram at 40 is invaluable. Radiologists can use this first image as a reference point for all future screenings. By comparing a new mammogram to the baseline from age 40, they can spot subtle changes that might otherwise be missed in dense tissue. This comparative analysis is a powerful tool. Without that initial picture, radiologists are essentially reading each new mammogram in a vacuum, making it more difficult to identify the early signs of a developing cancer. It’s like trying to spot a new crack in a wall without knowing what the wall looked like last year.
The types of breast cancer that tend to occur in younger women also play a role in these findings. Women in their 40s are more likely to be diagnosed with more aggressive forms of breast cancer, such as triple-negative and HER2-positive cancers. These cancers can grow and spread rapidly. A screening interval of two or three years might be sufficient for slower-growing cancers common in post-menopausal women, but for these aggressive subtypes, a year or two can make a world of difference. The first screening at 40 acts as an early warning system specifically designed to catch these fast-moving diseases at their most vulnerable stage. Dr. Sarah Thompson, an oncologist not directly involved with the study but familiar with its findings, explains, “We’ve long known that breast cancer in younger women can be biologically distinct and more virulent. This research underscores that our screening protocols need to account for that reality. That first mammogram isn’t just a formality; it’s our first and best chance to intercept these aggressive cancers before they gain momentum.”
Beyond the clinical data, the research also sheds light on the very human reasons why women might miss this critical appointment. Life at 40 is often a whirlwind of competing responsibilities. Many women are at the peak of their careers, caring for young children, and often looking after aging parents. In this hectic landscape, a preventative health screening can easily be pushed to the bottom of a very long to-do list. There’s also the factor of fear. The anxiety surrounding a potential cancer diagnosis can lead to avoidance, a psychological phenomenon where individuals steer clear of situations that might cause distress. Other barriers include a lack of flexible appointment times, difficulties with transportation, or simply not understanding the profound importance of this specific screening. Addressing these practical and emotional hurdles is now a major part of the public health challenge. The message needs to be clear: this appointment is different. It’s a unique opportunity that, if missed, carries a measurable cost.
The conversation around breast cancer screening has been complex and sometimes contradictory over the years. Different health organizations have varying guidelines, which can create confusion. Some recommend starting annual screenings at 40, while others suggest a baseline at 40 and then continuing every two years. This new evidence adds significant weight to the argument for not just starting at 40, but for ensuring high participation rates in that first round. It moves the discussion from “when should we start?” to “how do we ensure every woman has access to and attends her first screening?” Public health campaigns may need to be redesigned to target women in their late 30s, preparing them for the importance of this milestone. Healthcare providers are being encouraged to have more explicit conversations with their patients, explaining not just that they should get screened, but why this particular screening is so consequential for their future health.
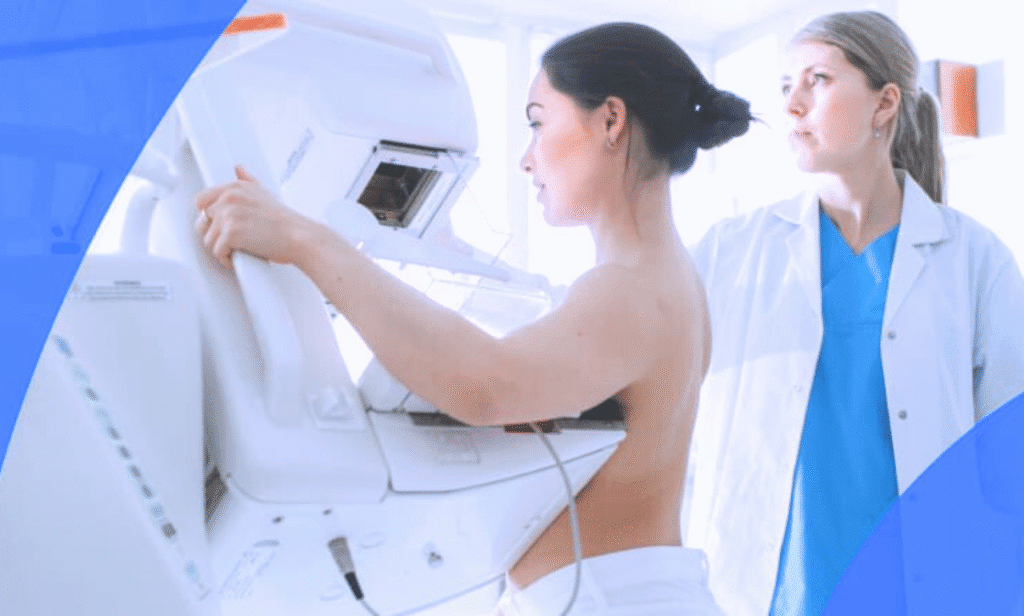
For any woman feeling anxious about her first mammogram, it’s helpful to know what to expect. The procedure itself is relatively quick, typically taking about 20 minutes. While the compression of the breast can be uncomfortable for a brief moment, it is a necessary step to get a clear image. The radiology technologist is trained to make the experience as comfortable as possible. The peace of mind that comes from a clear result, or the early detection of a treatable abnormality, far outweighs the momentary discomfort. The goal is to reframe the mammogram not as a source of fear, but as an empowering act of self-care. It is a proactive step that puts a woman in control of her health, leveraging modern medicine’s best tool for fighting breast cancer: early detection. This latest research makes it unequivocally clear that for women turning 40, prioritizing that first screening appointment is one of the most important health decisions they can make. It sets the stage for a lifetime of vigilant health management and dramatically alters the odds of survival should a cancer be present. The data speaks for itself: showing up for that first mammogram is a powerful defense against one of the most common cancers affecting women today.
