The female ovaries are remarkable, powerful organs about the size and shape of an almond. They are the cornerstone of the reproductive system, responsible for producing eggs for fertilization and secreting the essential hormones estrogen and progesterone. These hormones regulate the menstrual cycle, influence overall health, and support pregnancy. When something goes wrong with the ovaries, it can affect a woman’s health in profound and sometimes confusing ways. Understanding these potential problems is the first and most crucial step toward managing your health and seeking the right care. Many ovary issues share similar symptoms, which can make them tricky to self-diagnose, highlighting the importance of a professional medical opinion.
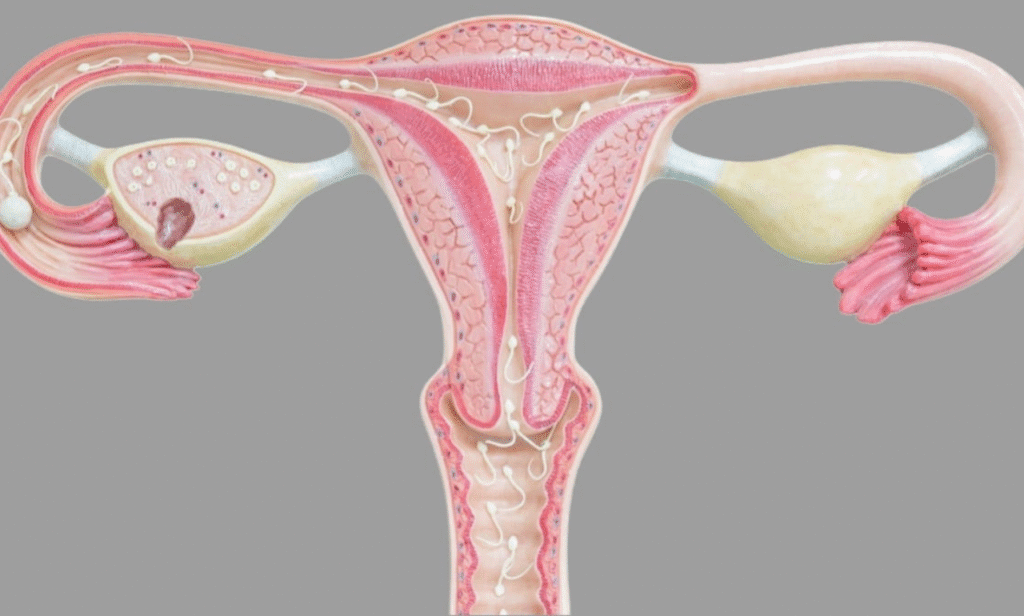
One of the most frequently diagnosed ovarian problems is the ovarian cyst. In simple terms, a cyst is a fluid-filled sac that forms on or inside an ovary. The vast majority of ovarian cysts are what doctors call “functional cysts.” These are a natural part of the menstrual cycle. Each month, a follicle cyst develops, which is the sac that holds a developing egg. This sac normally breaks open to release the egg and then dissolves. Sometimes, however, this process doesn’t go as planned. The sac might not release the egg and keep growing, becoming a follicular cyst. Or, after the egg is released, the sac, now called the corpus luteum, might not dissolve and instead seals up and fills with fluid, forming a corpus luteum cyst. These functional cysts are usually harmless, often don’t cause symptoms, and disappear on their own within a few menstrual cycles. The problem arises when cysts become large, rupture, or cause the ovary to twist, a painful condition known as ovarian torsion.
While most cysts are benign and resolve themselves, some can be more problematic. Conditions like endometriosis can lead to a specific type of cyst called an endometrioma, where tissue similar to the uterine lining grows on the ovaries. Another type, cystadenomas, develop from ovarian tissue and can be filled with a watery or mucous material; these can grow quite large. Dermoid cysts are bizarre but usually benign tumors that can contain tissue like hair, skin, or teeth because they form from embryonic cells. The symptoms of a problematic cyst can include pelvic pain, which might be a dull ache or a sharp, sudden pain if it ruptures, bloating, a feeling of fullness in the lower abdomen, and pain during intercourse. Diagnosis typically involves a pelvic exam and an ultrasound, which allows a doctor to see the cyst’s size, location, and composition. Treatment depends entirely on these factors, your age, and your symptoms. Often, a “watchful waiting” approach is adopted, with a follow-up ultrasound to see if the cyst shrinks. Birth control pills are sometimes prescribed to help prevent new cysts from forming in future cycles. For large, persistent, or painful cysts, laparoscopic surgery to remove the cyst may be recommended, a procedure that aims to preserve the ovary whenever possible.
Moving beyond cysts, a complex and common hormonal disorder affecting the ovaries is Polycystic Ovary Syndrome, or PCOS. It’s one of the most common endocrine disorders among women of reproductive age, affecting roughly one in ten women. The name is a bit misleading. Having PCOS does not mean you have “cysts” in the traditional sense. Instead, the “polycystic” appearance on an ultrasound refers to a large number of small, immature ovarian follicles that have gathered around the edge of the ovary, looking like a string of pearls. These are not harmful cysts but are follicles that have stalled in their development due to a hormonal imbalance. The core issues in PCOS are often insulin resistance and elevated levels of androgens, which are male hormones that females also produce in small amounts. This hormonal imbalance disrupts the menstrual cycle and prevents ovulation from occurring regularly. The symptoms of PCOS can be varied and far-reaching.
The classic signs of PCOS include irregular periods or no periods at all, difficulty getting pregnant due to lack of ovulation, excess hair growth on the face, chest, or back, weight gain or difficulty losing weight, and thinning hair on the head. Acne and oily skin are also common complaints. Because of the insulin resistance component, women with PCOS are at a higher risk for developing type 2 diabetes, high cholesterol, and heart disease later in life. Managing PCOS is a lifelong process focused on controlling symptoms and reducing long-term health risks. Treatment is highly individualized but often includes lifestyle modifications like a balanced diet and regular exercise to improve insulin sensitivity. Birth control pills can help regulate periods and reduce androgen-related symptoms like excess hair and acne. For those trying to conceive, medications like clomiphene or letrozole can be used to induce ovulation. Metformin, a drug commonly used for type 2 diabetes, is also sometimes prescribed to help manage insulin resistance in women with PCOS.
Another condition deeply intertwined with the ovaries is endometriosis. This is a disorder where tissue similar to the lining inside the uterus, called the endometrium, begins to grow outside the uterus. These implants can be found on the ovaries, the fallopian tubes, the outer surface of the uterus, and other organs within the pelvis. This tissue acts as it would inside the uterus—it thickens, breaks down, and bleeds with each menstrual cycle. However, because this tissue has no way to exit the body, it becomes trapped. Surrounding tissue can become irritated, eventually developing scar tissue and adhesions, which are bands of fibrous tissue that can cause pelvic tissues and organs to stick to each other. When endometriosis involves the ovaries, the trapped blood can form cysts called endometriomas or “chocolate cysts,” named for their dark, old blood content. The primary symptom of endometriosis is pelvic pain, often associated with menstrual periods. While many women experience cramping during their periods, those with endometriosis typically describe pain that is far worse than usual. The pain may also increase over time. Other symptoms include pain during or after sex, painful bowel movements or urination during periods, excessive bleeding, and infertility. An estimated twenty-five to fifty percent of infertile women have endometriosis. Diagnosis can only be confirmed through laparoscopy, a minor surgical procedure. Treatment options range from pain medication and hormone therapy to slow the growth of endometrial tissue to conservative surgery to remove the implants while preserving the uterus and ovaries.
A less common but more serious concern is ovarian cancer. It ranks fifth in cancer deaths among women and is often called a “silent killer” because symptoms are typically vague and easily attributed to other, more common conditions. This is why awareness is critical. The risk factors for ovarian cancer include a family history of the disease, inherited gene mutations like BRCA1 and BRCA2, increasing age, never having carried a pregnancy to term, and endometriosis. The symptoms are persistent and a change from a woman’s normal baseline. They can include bloating, pelvic or abdominal pain, difficulty eating or feeling full quickly, and urinary symptoms like urgency or frequency. It’s the persistence and combination of these symptoms that should prompt a visit to a doctor. If ovarian cancer is suspected, diagnostic tests may include a transvaginal ultrasound and a blood test for a marker called CA-125. However, these tests are not definitive for cancer, and a biopsy is required for a final diagnosis. Treatment almost always involves surgery to remove the cancerous tissue, which may include a hysterectomy and removal of both ovaries and fallopian tubes, followed by chemotherapy.
Primary Ovarian Insufficiency, also known as premature ovarian failure, is another challenging condition. It occurs when the ovaries stop functioning normally before a woman is forty. They stop producing normal amounts of estrogen and may not release eggs regularly. This is not the same as early menopause, as some women with POI may still have occasional periods and even get pregnant. The cause is often unknown but can be related to autoimmune diseases, genetic factors, or toxins from chemotherapy or radiation. The symptoms mirror those of natural menopause: irregular or skipped periods, hot flashes, night sweats, vaginal dryness, irritability, and difficulty concentrating. The low estrogen levels also increase the risk of osteoporosis. While there’s no proven treatment to restore normal ovarian function, therapies focus on managing the symptoms and protecting long-term health, often through hormone replacement therapy and calcium and vitamin D supplementation for bone health.
Recognizing the signs that something might be wrong is the most powerful tool a woman has. You know your body better than anyone. If you experience persistent pelvic pain, significant changes in your menstrual cycle, pain during intercourse, unexplained weight gain or loss accompanied by other symptoms, or any of the persistent signs associated with ovarian cancer, it is time to schedule an appointment with your gynecologist or healthcare provider. Do not dismiss your concerns. Keeping a symptom diary can be incredibly helpful for your doctor. Track your periods, the nature and timing of any pain, and any other changes you notice. When you go to your appointment, be prepared to discuss your personal and family medical history in detail. Your doctor will likely start with a pelvic exam. From there, diagnostic tools can include blood tests to check hormone levels, an ultrasound to get a clear picture of the ovaries, and in some cases, more advanced imaging or laparoscopy. The goal is always to find the root cause of the problem so that an effective, personalized treatment plan can be created. This plan will consider your symptoms, your age, your overall health, and your future fertility goals. Managing ovary problems is a partnership between you and your doctor, built on open communication and a shared goal of achieving and maintaining your best possible health.
