Health officials in California are tracking a noticeable increase in mpox infections, a development that has sparked concern about a potential resurgence of the virus. This new cluster of cases, primarily concentrated in the San Francisco Bay Area, serves as a stark reminder that the threat of mpox has not vanished. The outbreak underscores the critical importance of sustained vaccination efforts and public awareness, particularly within the communities most affected. While the massive global outbreak from 2022 has significantly receded, the virus continues to circulate at low levels. This recent uptick in California is a clear signal that public health agencies and the public cannot afford to become complacent. The situation is being monitored closely to prevent the kind of rapid spread witnessed previously.
The current cases in California share a familiar profile with the 2022 outbreak, predominantly affecting men who have intimate contact with other men. This pattern reinforces the understanding that mpox spreads through prolonged, close, and often skin-to-skin contact. The virus is not a disease exclusive to any one group, but it has found a particular foothold in specific social and sexual networks. Transmission typically occurs through direct contact with the infectious rash, scabs, or bodily fluids of an infected person. It can also spread by respiratory secretions during prolonged face-to-face contact, or by touching items like clothing or bedding that have previously been touched by the rash. Understanding these transmission routes is fundamental to prevention and control, helping individuals assess their own level of risk accurately.
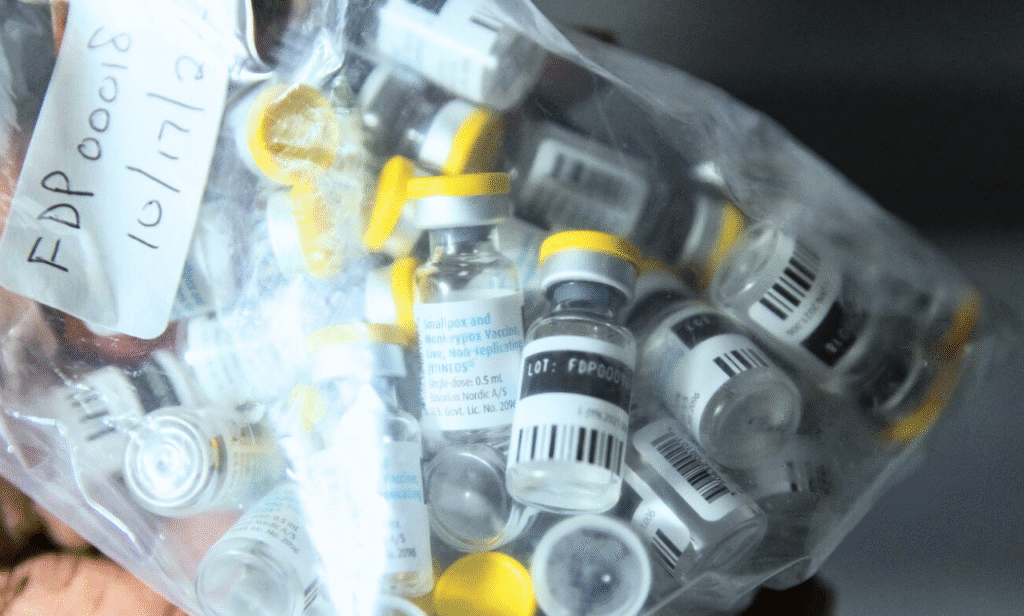
A significant factor in this new California cluster appears to be a large number of individuals who were eligible for the mpox vaccine but never received it. Many of the recently infected people were either unvaccinated or had only received one dose of the two-dose JYNNEOS vaccine regimen. This highlights a dangerous gap in protection. The vaccine is a powerful tool for preventing infection or, in breakthrough cases, making the illness much milder. Public health experts point to this as a classic example of a prevention wall; when a sufficient portion of an at-risk community is vaccinated, it breaks chains of transmission and protects everyone. The current situation suggests that this wall has developed some cracks due to lagging vaccination rates.
The symptoms of mpox remain consistent with what was documented during the larger outbreak. The most recognizable sign is a rash that can look like pimples or blisters. This rash may be painful or itchy and goes through several stages, including scabs, before healing. The rash can be located on or near the genitals or anus but could also appear on the hands, feet, chest, face, or mouth. Other symptoms often include fever, chills, swollen lymph nodes, exhaustion, muscle aches, and headache. These flu-like symptoms sometimes precede the rash, but the rash can also appear first. Crucially, symptoms can sometimes be very mild, perhaps just a single lesion, which can be mistaken for another condition. This makes awareness and testing all the more important.
For those who do contract the virus, the experience can vary widely. Some people have a very mild illness with only a few lesions, while others may experience a more severe, painful rash and significant systemic symptoms. The reason for this variation can depend on a person’s overall health and, most importantly, their vaccination status. Individuals who are immunocompromised, including those with advanced HIV, have a higher risk of developing severe illness if they become infected with mpox. This is a key point of concern for health providers, who emphasize the need for extra protection for these vulnerable individuals. The majority of hospitalizations and deaths during the 2022 outbreak were among people with severely weakened immune systems.
The public health response in California has been swift and targeted. Health departments are ramping up their outreach efforts, using social media, community organizations, and healthcare providers to get the message out about the new cases. They are strongly urging anyone who is at risk, especially those with multiple sexual partners or who attend events where intimate contact may occur, to complete their two-dose vaccination series. Free and low-cost vaccines are available at many public health clinics and through specific healthcare partners. The strategy is to create a ring of immunity around the outbreak to contain it before it can spread more widely. This approach requires strong collaboration between health officials and community leaders.
Testing is another critical component of the containment strategy. Anyone who develops a suspicious rash or other symptoms consistent with mpox should seek medical attention and get tested immediately. Early diagnosis allows for prompt isolation, which helps prevent spreading the virus to others. It also enables people to access treatments if needed. The antiviral medication tecovirimat, or TPOXX, is available for individuals with more severe disease or who are at high risk for complications. This treatment can help shorten the duration of the illness and alleviate suffering. Doctors are being reminded to consider mpox in their diagnoses and to order tests without stigma or hesitation.
The global context of mpox is also relevant. While cases have dropped dramatically worldwide, the virus remains endemic in several Central and West African countries. The international travel and interconnectedness of the modern world mean that an outbreak in one region can quickly seed cases in another. The California cluster is a domestic example of how a virus can simmer and then flare up when conditions are right. Continuous global surveillance and data sharing are essential for tracking the evolution of the virus and understanding any potential changes in its transmissibility or severity. Scientists are still learning about mpox and its long-term implications.
The economic and social impact of a resurgent mpox outbreak should not be underestimated. During the 2022 crisis, many people faced weeks of isolation, lost wages, and significant medical expenses. The emotional toll of dealing with a painful illness and the associated stigma was also profound. Preventing another large-scale outbreak is not just a public health imperative but a social and economic one as well. Investing in vaccination campaigns and public education is far more cost-effective than managing a widespread health emergency. It also protects the healthcare system from being overwhelmed by another infectious disease.
Looking ahead, the trajectory of mpox in California and beyond will depend heavily on the actions taken now. The goal is to move from an emergency response to a sustainable, long-term management strategy. This means integrating mpox prevention into routine healthcare services, such as sexual health clinics and primary care offices. Normalizing the mpox vaccine as part of standard preventive care for at-risk individuals is a key objective. The lessons learned from the HIV epidemic and the COVID-19 pandemic about the importance of community trust and equitable access to resources are directly applicable to the ongoing mpox situation.
Personal responsibility plays a vital role in this public health effort. Individuals need to stay informed about the current risk level in their area. They should assess their own personal risk based on their behaviors and social networks. Getting vaccinated if eligible is the single most powerful action a person can take to protect themselves and their community. Being aware of the symptoms and seeking testing promptly if they appear is another critical piece. Open conversations with healthcare providers and intimate partners about health and prevention can help reduce stigma and encourage safer practices. Collective action stems from individual choices.
The development and deployment of effective vaccines have fundamentally changed the landscape of the mpox threat. The JYNNEOS vaccine has proven to be a safe and effective countermeasure. Research from the 2022 outbreak showed that even one dose offered a significant level of protection, but two doses are considered essential for robust and durable immunity. The vaccine can be used in two ways: to prevent infection in someone who has been exposed but is not yet showing symptoms, and as a routine preventive measure for those at ongoing risk. Understanding the different use cases for the vaccine helps demystify it and encourages broader uptake.
For public health communicators, the challenge is to keep mpox on the public’s radar without causing panic. The message is one of cautious vigilance. The tools to control the virus exist, but they only work if people use them. The recent cases in California are a warning, but they are also an opportunity. They provide a chance to re-engage with prevention efforts, to close the vaccination gap, and to strengthen the public health infrastructure. By learning from this recent cluster, other regions can also bolster their own surveillance and readiness, ensuring a coordinated defense against a potential wider resurgence of mpox. The path forward requires persistence, partnership, and a clear-eyed view of the ongoing risk.
