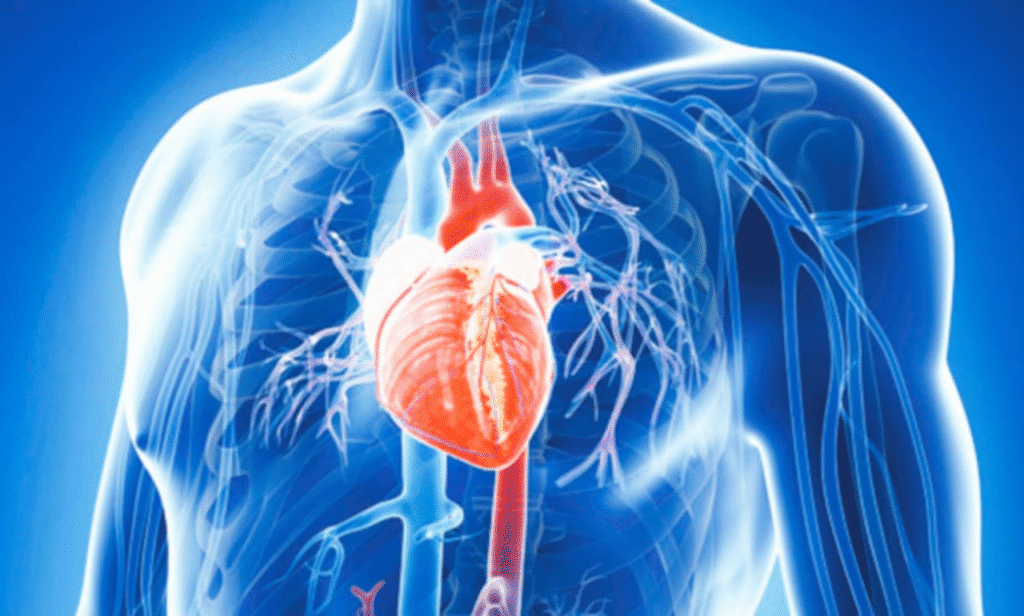
An aortic aneurysm is one of those conditions that earns the title “silent killer” for good reason. It hides in plain sight, often developing quietly without warning, while millions of people continue with their daily lives unaware of the risk sitting inside their chest or abdomen. The aorta is the body’s main artery, carrying oxygen-rich blood from the heart to every part of the body. When a weakness forms in its wall, it can balloon outward like a fragile bubble. At first, this ballooning may cause no pain and no obvious symptoms. Yet, if it grows too large or bursts, the result can be catastrophic, often fatal within minutes.
Medical experts in the United States have repeatedly raised concerns about this condition, pointing out how it affects far more people than most realize. In fact, it’s estimated that about one percent of the population has an aortic aneurysm at any given time, though the majority do not know it. Because symptoms are often absent, many only learn about it after undergoing a scan for something else, or tragically, when it ruptures without warning. Statistics show that nearly 10,000 people in America die each year from an aortic aneurysm rupture, highlighting why awareness and screening matter so much.
To understand this condition better, it helps to picture the structure of the aorta. Imagine a thick garden hose connected to a pump. If one part of the hose wall weakens, pressure inside forces it to bulge. At first, the bulge might not interfere with water flow. But the longer the pressure builds, the more the risk grows that the hose will split. That’s exactly what happens in the body when the aortic wall weakens. Unlike a garden hose, though, you can’t replace the aorta easily, and a rupture can lead to life-threatening internal bleeding in seconds.
There are two main types of aortic aneurysms: thoracic, which occur in the chest portion of the aorta, and abdominal, which occur in the section running through the belly. Both carry risks, but abdominal aortic aneurysms are more common, particularly in men over the age of sixty-five. Men who have smoked at any point in their lives face an especially high risk. Smoking damages the arteries and accelerates weakening, making aneurysm formation more likely.
The tricky part about aortic aneurysms is that they rarely send clear warning signals in their early stages. Some people may experience vague abdominal or back discomfort, but it’s often dismissed as indigestion, muscle strain, or simple fatigue. Others may notice a pulsing feeling in the stomach, especially when lying down, but again, it is easy to ignore. Because these signs are nonspecific, the majority of cases go undiagnosed until a scan is performed. When symptoms do appear suddenly and strongly, it often means the aneurysm is close to rupturing. Severe pain in the chest, abdomen, or back, dizziness, rapid heartbeat, fainting, or even shock are red flags of an emergency situation.
Risk factors extend beyond smoking. High blood pressure is another major culprit. Constantly elevated pressure inside the arteries stresses the vessel walls, making them more likely to bulge. Atherosclerosis, or the buildup of fatty deposits inside arteries, also weakens the aortic wall. Family history plays a significant role too. If a parent, sibling, or close relative had an aneurysm, the likelihood of inheriting the tendency increases. Certain genetic conditions, such as Marfan syndrome or Ehlers-Danlos syndrome, can also predispose individuals because they affect connective tissue strength.
Doctors emphasize that early detection can mean the difference between life and death. Screening through ultrasound or CT scans allows physicians to see if the aorta is enlarging before it becomes dangerous. In the United States, the Preventive Services Task Force recommends that men aged sixty-five to seventy-five who have smoked at any point undergo at least one abdominal ultrasound. For those with family history or other risk factors, earlier screening may be advised. Women are less likely to develop aneurysms, but when they do, outcomes are often worse, making vigilance equally important.
Once an aneurysm is detected, management depends on its size and growth rate. Small aneurysms, typically under 5 centimeters, may simply be monitored with regular imaging every six months to a year. During this watchful waiting period, lifestyle changes are crucial. Quitting smoking, controlling blood pressure, eating a heart-healthy diet, and exercising moderately all slow the growth of the aneurysm. Larger aneurysms or those growing rapidly require medical intervention. Surgeons may perform open repair, replacing the damaged section of the aorta with a synthetic graft, or they may use a less invasive procedure called endovascular aneurysm repair (EVAR), where a stent graft is inserted through a catheter to reinforce the weak spot from within.
Both procedures have saved countless lives, but timing is key. A rupture carries a survival rate of less than 20 percent, while elective repairs performed before rupture often have excellent outcomes. This is why awareness, regular checkups, and proactive management matter so much. Patients who undergo elective repair typically recover well and return to their normal lives with improved long-term survival.
Numbers underline the seriousness of this silent threat. Globally, the burden is heavy, with thousands dying each year due to undiagnosed or untreated aneurysms. In the United States, about 200,000 people are diagnosed with abdominal aortic aneurysm annually, and thousands more remain undiagnosed. Worldwide, aneurysms account for significant health care costs, emergency interventions, and loss of life. And yet, because the condition is so quiet, public awareness remains surprisingly low. Heart disease, stroke, and cancer receive much more attention, leaving aneurysms in the shadows.
One case that illustrates this is that of a 68-year-old man, a former smoker with a history of high blood pressure. He had no symptoms but went for a routine check-up, where his doctor ordered an ultrasound. The scan revealed a 5.5-centimeter abdominal aneurysm, which was promptly repaired with a stent graft. He made a full recovery and continued enjoying his retirement. Contrast this with another patient who ignored persistent back pain, assuming it was age-related. He collapsed suddenly due to a rupture, and despite emergency surgery, he did not survive. These examples highlight the difference early detection makes.
Preventing aneurysms starts with controlling the risk factors that damage blood vessels. Quitting smoking tops the list. Research shows that smoking increases the risk of abdominal aortic aneurysm up to five times. Blood pressure control through lifestyle or medication is another cornerstone. Eating a diet low in saturated fats and high in fruits, vegetables, and whole grains supports vascular health. Regular exercise strengthens the heart and helps manage weight. Even stress management plays a role, since chronic stress can elevate blood pressure.
Education is also key. People need to know that aneurysms exist, that they are silent, and that screening is available. Public health campaigns in some countries have already reduced aneurysm deaths by encouraging at-risk populations to get screened. In the UK, for example, men aged sixty-five receive an invitation for a free ultrasound scan. Similar efforts in the US and other nations could prevent thousands of unnecessary deaths each year.
The medical community also stresses the importance of individualized care. Not every aneurysm requires surgery, and not every patient is the same. Doctors weigh factors such as age, overall health, aneurysm size, and growth rate before recommending treatment. Advances in surgical techniques, particularly minimally invasive endovascular procedures, have broadened options and reduced recovery times. Patients today have better chances than ever before—provided the aneurysm is found in time.
Research continues into the genetic and molecular underpinnings of aneurysms. Scientists are studying how inflammation, enzymes, and cellular signaling contribute to weakening of the aortic wall. New drugs may one day help stabilize aneurysms and prevent growth without the need for surgery. For now, though, the most effective tools remain early detection, lifestyle management, and timely surgical intervention when necessary.
Ultimately, an aortic aneurysm represents both a challenge and an opportunity. The challenge lies in its stealth, its ability to grow unnoticed, and its deadly potential if ruptured. The opportunity lies in the fact that it can be detected with a simple, painless scan. It can be managed with lifestyle adjustments and, if needed, treated successfully with surgery. By raising awareness, promoting screening, and encouraging healthy living, the medical community aims to turn the tide against this hidden killer.
For individuals, the takeaway is straightforward. If you fall into a risk category—over sixty, smoker, high blood pressure, or family history—speak to your doctor about screening. Pay attention to unusual symptoms, even if they seem minor. Live in a way that supports vascular health, with good food, regular movement, and no tobacco. These steps not only protect against aneurysms but also against a wide range of cardiovascular diseases.
The silent nature of this condition should not mean silent action. Every conversation, every check-up, every lifestyle change adds to the prevention of tragedy. With greater awareness and proactive health care, countless lives can be saved from the sudden and devastating impact of aortic aneurysm rupture.
