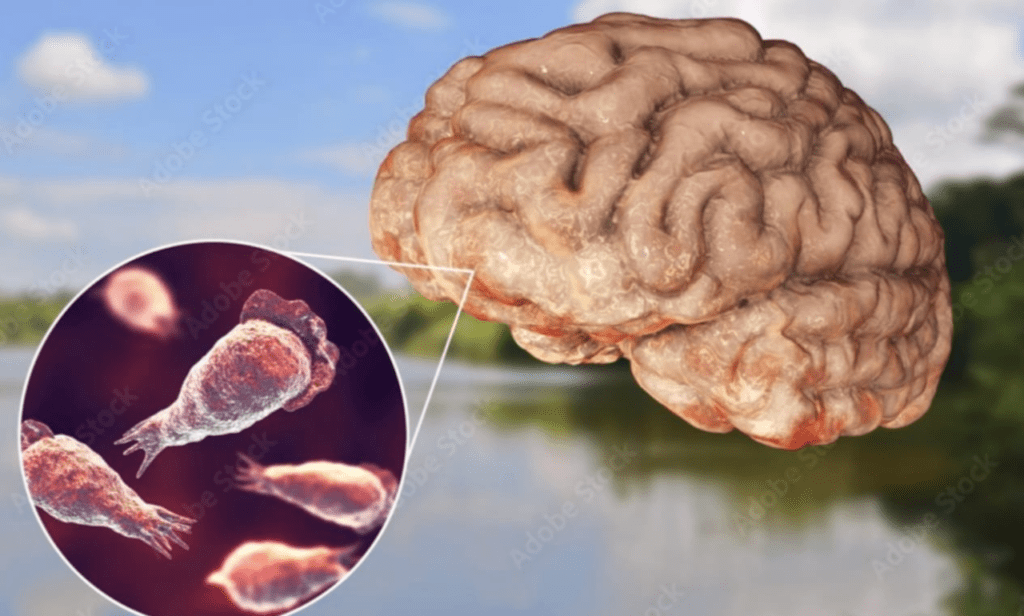
Health authorities recently confirmed a tragic death caused by Naegleria fowleri, a microscopic brain-eating amoeba, following exposure in a warm southern lake. This devastating but exceptionally rare infection occurs when contaminated water enters the nose during swimming, diving, or water sports. The amoeba migrates along olfactory nerves to the brain, sparking a ferocious inflammatory attack known as Primary Amebic Meningoencephalitis (PAM). Within days, this destroys brain tissue with alarming speed. The case has reignited urgent discussions about freshwater safety as summer temperatures climb.
Understanding Naegleria fowleri requires examining its natural behavior. This single-celled organism thrives in warm, stagnant freshwater environments, particularly lakes, hot springs, and poorly maintained ponds where temperatures exceed 80°F (27°C). Unlike bacteria or viruses, it doesn’t seek human hosts; infection occurs accidentally when forceful water entry propels it into the nasal passages. Climate scientists note expanding risk zones as regional temperatures rise, with recent cases appearing in historically cooler states like Minnesota and Indiana. Drought conditions compound dangers by concentrating amoebae populations in shallow, receding shorelines where swimmers often congregate.
Initial symptoms present a diagnostic nightmare. Between one and nine days post-exposure, patients develop sudden fever, explosive headaches, and nausea, mimicking common viral illnesses. This overlap delays critical testing, allowing the amoeba to advance unchecked. By day five, neurological deterioration accelerates: confusion, seizures, neck stiffness, and hallucinations signal irreversible brain swelling. Mortality rates exceed 97%, largely because most cases are identified too late for intervention. Since 1962, only four of 157 U.S. victims survived. One survivor, Kali Hardig, contracted PAM at age 12 in Arkansas; her unprecedented recovery involved experimental hypothermia therapy and the drug miltefosine, now stocked by major hospitals in high-risk regions.
Treatment protocols remain agonizingly limited. Once PAM develops, neurologists deploy amphotericin B (an aggressive antifungal) alongside antibiotics like azithromycin. Miltefosine—originally developed for breast cancer—shows promise by disrupting amoeba cell membranes, but must be administered within 72 hours of symptom onset. “This infection moves faster than our diagnostics,” explains CDC epidemiologist Dr. Julia Haston. “By the time spinal fluid confirms amoebic presence, patients are often comatose.” Current research explores rapid nasal swab tests and early immune biomarkers to buy precious hours.
Prevention hinges on practical behavioral adjustments. Health departments emphasize nose protection as the single most effective defense. Nose clips—common among competitive swimmers—block water intrusion during diving or underwater activities. Additional safeguards include avoiding sediment disturbance in warm shallows, keeping heads above water in hot springs, and opting for flowing rivers over stagnant ponds. Crucially, swallowing contaminated water poses zero risk; infection requires nasal entry. Properly chlorinated pools and treated municipal water remain safe, as chlorine kills amoebae within seconds.
The psychological impact on affected communities runs deep. Following this southern lake incident, authorities temporarily closed access for testing, though no additional amoebae were detected. Similar closures occurred after recent fatalities: a Nevada boy exposed at Lake Mead in 2022, and two Florida cases linked to private ponds last summer. “We balance transparency against unnecessary panic,” says local health director Marcus Reynolds. “While statistically rarer than lightning strikes, one preventable death warrants clear public guidance.” Survivor Kali Hardig advocates nationally for standardized emergency protocols: “Every hospital near recreational waters needs miltefosine on hand. My life was saved because Arkansas Children’s Hospital acted immediately.”
Geographic shifts in cases reveal climate connections. Historically confined to southern states, Naegleria fowleri now appears farther north. A 2023 Iowa case followed record heat waves, while Nebraska’s first infection coincided with prolonged drought. Researchers attribute this to warmer seasonal water temperatures persisting into autumn months. However, water testing remains impractical—amoebae concentrations vary daily, and no rapid field tests exist. Instead, agencies prioritize education: “If you experience sudden, crushing headaches after freshwater exposure, demand specific PAM screening,” urges Dr. Reynolds. “Mention the water activity explicitly to emergency staff.”
Debunking myths remains essential. Unlike fictional parasites, Naegleria fowleri cannot infect through skin contact, drinking water, or aerosolized droplets. Saltwater environments naturally neutralize the organism. While social media occasionally fuels unwarranted fears, documented cases average fewer than three annually nationwide—a stark contrast to 4,000 annual drowning deaths. Still, experts stress that low probability doesn’t negate preparedness. Families planning lake activities should learn PAM’s early signs and locate hospitals stocking miltefosine via the CDC’s treatment network.
Innovations offer glimmers of hope. University researchers are engineering nanoparticle treatments that target amoebae without harming brain cells. Australia—where warmer climates see higher exposure—pilots AI-assisted beach sensors that estimate amoeba risk using temperature, turbidity, and rainfall data. Meanwhile, improved survivor outcomes hinge on public awareness. As temperatures soar, health departments nationwide reinforce the same message: Enjoy summer waters, but guard your nose. That simple barrier could mean the difference between life and catastrophic loss.
