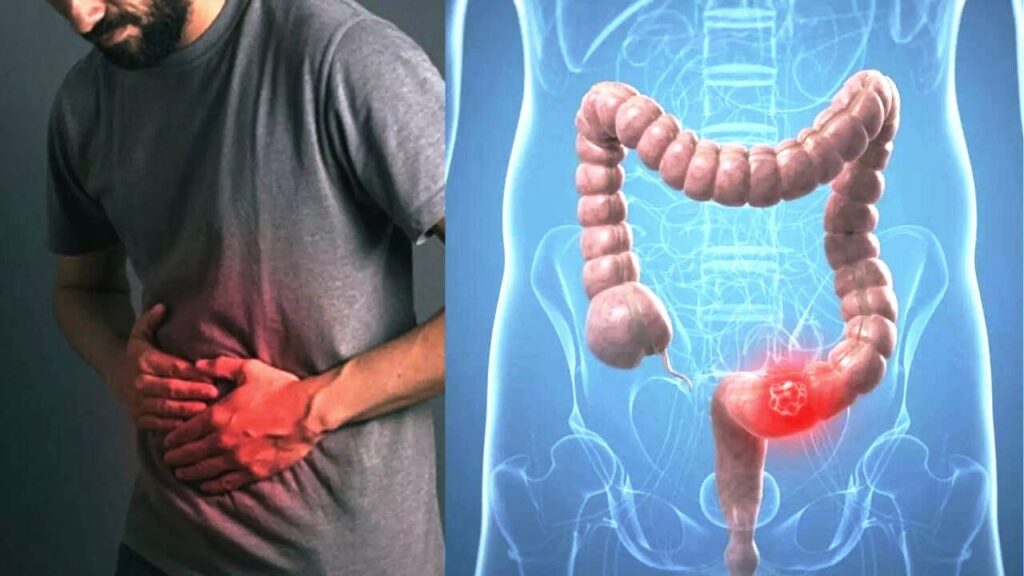
Colon cancer, often referred to as colorectal cancer when it involves both the colon and the rectum, is one of the most significant health concerns around the globe. This disease occurs when abnormal cells develop in the lining of the large intestine, eventually forming polyps that can transform into malignant tumors if they remain undetected or untreated. People who are diagnosed with colon cancer may experience a wide array of physical symptoms, yet many individuals remain entirely asymptomatic in the initial stages, making regular screenings a crucial aspect of prevention. Although medical research on colon cancer has grown tremendously in recent decades, there is still a degree of misinformation and confusion surrounding its causes, risk factors, and effective treatment strategies. Understanding the fundamental aspects of colon cancer can empower people to make well-informed decisions about their health and encourage timely screening and intervention measures. This educational exploration of colon cancer addresses everything from initial development and signs to risk management, diagnostics, and treatment possibilities, shedding light on how lifestyle and genetics both play integral roles.
The colon, also known as the large intestine or large bowel, is responsible for reabsorbing fluids and processing waste material, eventually preparing it for elimination. Because this part of the digestive system handles an extensive volume of material and interacts with countless microorganisms, it is especially susceptible to cellular changes that can lead to cancer. Generally, colon cancer begins as a polyp—an abnormal growth that emerges from the inner lining of the intestine. These polyps vary in type and potential for malignancy. Adenomatous polyps, for instance, are considered pre-cancerous because they have a higher likelihood of developing into colon cancer over time. While having polyps does not guarantee a cancer diagnosis, it raises the stakes considerably. This is why routine screenings like colonoscopies can help detect and remove these growths before they become a significant threat to health.
Age is often a defining factor in colon cancer risk. Historically, medical guidelines have recommended that individuals start routine screening at age 50, but more recent trends show a rise in younger-onset colon cancer. Consequently, many health organizations now advise initiating routine screening at age 45. Despite this general recommendation, it’s critical to acknowledge that risk varies widely from person to person based on factors like family history, overall health status, and lifestyle choices. Family history is particularly relevant: if a close relative (parent, sibling, or child) has had colon cancer, the risk nearly doubles. Certain hereditary conditions, such as Lynch syndrome (Hereditary Nonpolyposis Colorectal Cancer) or Familial Adenomatous Polyposis, can increase the risk of developing colon cancer at a younger age and often necessitate earlier, more frequent screenings.
In addition to age and genetics, lifestyle factors significantly influence the likelihood of developing colon cancer. Diet is one of the most studied aspects. People who consume high amounts of red and processed meats have demonstrated higher incidences of colon cancer, in contrast to those who emphasize plant-based diets rich in fiber, whole grains, vegetables, and fruits. While the relationship between diet and colon cancer risk remains complex, many researchers believe that the pro-inflammatory properties of certain foods may play a contributing role in initiating or accelerating abnormal cell growth. Obesity also stands out as a considerable risk factor for colon cancer, potentially due to the metabolic and hormonal changes it introduces. Meanwhile, a sedentary lifestyle can compound this effect, indicating the protective value of regular exercise. Physical activity helps maintain healthy body weight and may also aid in regulating intestinal transit, thereby reducing the contact time between potential carcinogens and the colon.
Symptoms of colon cancer, when they appear, can vary widely and sometimes overlap with other digestive conditions. Among the most common indicators are persistent changes in bowel habits, such as diarrhea or constipation that doesn’t resolve within a few days. Individuals might also notice rectal bleeding or the presence of blood in their stool, which can appear as bright red streaks or as darker, tar-like discolorations. Abdominal discomfort, such as persistent cramping, bloating, or a feeling that the bowel has not emptied completely, can also hint at possible issues in the colon. Unexplained weight loss is another critical sign. Because colon cancer can impair the body’s ability to properly absorb nutrients while ramping up metabolic processes in cancer cells, patients may lose weight without any clear reason. Fatigue, resulting from either chronic blood loss in the stool or cancer’s effects on the body, is yet another red flag. Still, these symptoms can mimic those of less severe conditions, making it vitally important to consult a healthcare professional and undergo proper testing rather than self-diagnose.
Screening and early detection remain among the most potent weapons against colon cancer. There are a variety of tests available, ranging from non-invasive stool-based assessments to more direct visualization techniques. A fecal immunochemical test (FIT) involves checking the stool for hidden traces of blood. While non-invasive, it is typically repeated each year to optimize early detection. Meanwhile, a colonoscopy is considered the gold standard for detecting and removing polyps. During this procedure, a specialist uses a flexible tube equipped with a camera (a colonoscope) to visually inspect the entire colon. If polyps are found, they can often be removed on the spot, thus preventing possible malignant transformations. Virtual colonoscopy, which employs CT scanning, offers a less invasive look at the colon’s interior but does require additional testing or a standard colonoscopy if any suspicious areas are identified. Additionally, there are newer DNA-based stool tests designed to detect specific genetic changes in the cells that might be shed by tumors or polyps. Some physicians may suggest combining different screening approaches, especially for individuals with higher risk profiles.
Once colon cancer is diagnosed, staging the disease becomes paramount. Stages typically range from I through IV, with each step reflecting how far the cancer has spread. In Stage I, cancer is confined to the inner layers of the colon. By Stage II, it has penetrated deeper layers but remains localized. Stage III usually indicates that the cancer has spread to nearby lymph nodes, while Stage IV signifies that it has reached distant organs like the liver or lungs. Accurately determining the stage is crucial because it guides treatment planning. Imaging tests, such as CT scans or MRI, alongside biopsies, help determine precisely how far the cancer has progressed. The specific cell types and genetic markers found in biopsy samples can also offer valuable insights into how the tumor might respond to targeted treatments.
Treatment for colon cancer often depends on factors including the stage, tumor characteristics, and the patient’s overall health status. Surgery is frequently the first line of defense, especially if the cancer is diagnosed in an earlier stage. In these cases, surgeons typically remove the affected segment of the colon, along with nearby lymph nodes, to minimize the risk of residual cancer cells. Following surgery, patients may or may not need additional therapies. In more advanced stages, or if there is a higher risk of recurrence, chemotherapy can be administered to destroy cancer cells that may have spread beyond the primary site. Chemotherapy drugs can be given orally or through intravenous infusions, often in multiple cycles. Another layer of treatment includes radiation therapy, which is more commonly used for rectal cancer but can be an option in certain colon cancer scenarios, particularly when the tumor is found in areas that allow for targeted radiation.
Targeted therapies, such as monoclonal antibodies and drugs that inhibit specific molecular pathways, have emerged as promising options in the treatment of colon cancer. These medications focus on blocking the growth signals cancer cells need or preventing the formation of new blood vessels that sustain tumor growth. Immunotherapy, which harnesses the immune system to identify and destroy cancer cells, has also shown progress in certain cases, especially those that exhibit genetic markers like high microsatellite instability. For patients who are not surgical candidates or whose cancer has metastasized extensively, palliative treatments aim to relieve symptoms and maintain quality of life. These might include procedures that alleviate blockages in the colon or targeted radiation to reduce tumor size and alleviate pain.
Throughout the treatment process, the role of supportive care should not be underestimated. Emotional well-being, mental health, and practical daily living considerations all come to the forefront. Many individuals benefit from joining support groups, whether in-person or online, where they can interact with others who have undergone or are currently undergoing treatment. Diet and exercise also play a role in supporting recovery and overall health, under the guidance of healthcare professionals who can tailor recommendations to the patient’s condition and tolerance levels. Nutritional advice might include ensuring adequate protein intake to support tissue repair, focusing on nutrient-rich foods, and staying hydrated. Physical activity, such as mild to moderate exercises recommended by a physician, can improve mood and energy levels, in addition to assisting in the body’s ability to handle treatments.
When people consider the role of genetics in colon cancer, they may worry about familial risks. Although having a close family member diagnosed with colon cancer can raise an individual’s susceptibility, lifestyle still wields considerable influence over disease outcomes. Moreover, genetic tests are available for identifying inherited conditions like Lynch syndrome. These tests can help families craft more proactive screening schedules, as detecting polyps at an earlier stage can be a game-changer. Even individuals without a strong family history sometimes choose to pursue genetic counseling if there are other red flags, such as a personal history of multiple cancers or early diagnoses in distant relatives. Such measures offer an additional layer of vigilance and education.
Preventive strategies for colon cancer converge on a few core principles: routine screening, a balanced diet, regular physical activity, and awareness of personal and family medical history. For those looking to make diet improvements, focusing on high-fiber foods like whole grains, beans, and a variety of colorful fruits and vegetables is frequently encouraged. Emphasizing lean proteins from fish and plant-based sources can also be beneficial, along with minimizing processed and red meats. Meanwhile, limiting alcohol consumption and avoiding tobacco are standard guidelines for reducing the risk of many cancers, including those of the colon. Because obesity is consistently linked with higher rates of colon cancer, weight management via a balanced calorie intake and exercise regimen can serve as another protective measure.
While biology plays a central role in colon cancer development, the environment often exerts a powerful influence. Chronic stress, for instance, has been explored as a potential risk factor due to its effects on the body’s inflammatory responses and immune regulation. However, research in this area remains a work in progress, and most clinicians will emphasize proven risk factors like diet, exercise, and genetic predisposition. Nonetheless, fostering good mental health through stress reduction techniques, therapy, or mindfulness programs can still have a positive impact on overall well-being. This holistic approach can be especially beneficial for individuals who are in higher-risk categories and want to do everything in their power to stay healthy.
Medical advancements continue to reshape the way colon cancer is detected and treated. Liquid biopsies, which involve analyzing blood samples for cancer markers, are currently being studied to see if they can detect colon cancer in its earliest stages. Robotic-assisted surgeries are becoming increasingly refined, offering precise removal of cancerous tissue with potentially quicker recoveries. Researchers are also exploring new immunotherapy agents, in hopes of delivering more targeted treatments that yield fewer side effects than chemotherapy. Furthermore, public health campaigns have worked to expand awareness of colon cancer across demographics, aiming to combat taboos and encourage screenings among individuals from diverse backgrounds. Early detection remains the key to improving survival rates, and educational initiatives underscore the simplicity and importance of screening tests.
Patients diagnosed with colon cancer can benefit from a multidisciplinary approach to treatment. Oncologists, surgeons, radiation specialists, nutritionists, and mental health professionals come together to address the various facets of the disease. This team-based strategy ensures that the patient’s physical, emotional, and social needs are met. Continual follow-up appointments remain essential after initial treatment. Healthcare providers monitor for recurrence through imaging tests and colonoscopies, because colon cancer can reappear if even a few malignant cells survive treatment. During these follow-ups, additional health complications can be addressed, and lifestyle recommendations can be revised to meet new needs.
The emotional toll of a colon cancer diagnosis can be immense, both for patients and their loved ones. Many treatment centers now integrate psychological counseling and social work support into their standard care plans, recognizing that mental health is closely linked with successful treatment outcomes. Anxiety and depression are relatively common, especially during the uncertainty of long treatment cycles. Individual therapy or group support sessions can provide tools to cope with these challenges, as can mindfulness-based stress reduction techniques. Loved ones and caregivers also need resources and guidance, because they shoulder a range of responsibilities—from helping with medical appointments to assisting with daily tasks—and can be susceptible to burnout.
Among the many misconceptions that exist about colon cancer, one is that it exclusively affects older men. While historically this demographic was at a higher risk, the disease can and does affect a variety of age groups and sexes. In fact, there has been a documented rise in colon cancer among younger adults in recent years, prompting medical bodies to lower the recommended screening age and encourage discussions about digestive health symptoms among healthcare providers. Another misconception is that a vegetarian or vegan diet completely eliminates colon cancer risk. Although plant-based diets can be protective, they do not guarantee immunity. Genetics, environmental exposures, and other variables still play a role. Hence, even those who follow seemingly healthy lifestyles should remain vigilant about screenings and be mindful of any concerning symptoms.
It’s also worth noting that not everyone who develops colon cancer has obvious risk factors. Some people may have none of the typical flags—no family history, no obesity, no poor diet—yet still receive a diagnosis. This reality underscores the necessity of routine screenings and open communication with healthcare providers. If someone experiences prolonged changes in bowel habits or unexplained gastrointestinal discomfort, a thorough check-up is warranted. It’s easy to attribute stomach or bowel issues to stress or dietary fluctuations, but persistent problems should not be ignored. With colon cancer, timing matters immensely. Polyps can take years to transform into invasive tumors, which is why removing them during early detection efforts can avert potentially life-threatening complications.
During active treatment, patients often wonder what they can do to support their bodies. Each individual’s journey will differ, and healthcare professionals can offer personalized guidelines. Nonetheless, maintaining a stable, balanced diet remains a foundational element. Whether someone is undergoing chemotherapy, radiation, or surgery, the body requires nutrients to mend tissues and maintain a robust immune response. Adequate hydration is equally important, especially if side effects include diarrhea or vomiting. Some patients find it helpful to keep a food journal, noting how certain meals affect their energy levels or digestive comfort. This helps in tailoring meals to maximize nutrient intake while reducing discomfort. In some cases, nutritional supplements or specialized shakes may be recommended, especially if appetite is limited or weight loss is a concern.
Exercise regimens should be tailored to an individual’s capabilities and treatment plan. Low-impact activities like walking, gentle yoga, and swimming can offer cardiovascular benefits and help reduce stress. People in the midst of chemotherapy might feel fatigued, and pushing beyond their physical limits could hinder recovery. Therefore, a realistic approach—perhaps a short daily walk or gentle stretches—can be more beneficial than a strenuous workout schedule. As treatments progress and the body adapts, the exercise program can be modified accordingly. Some medical centers provide specialized oncology rehabilitation programs that develop personalized exercise and nutrition plans for patients, ensuring safety and fostering better outcomes.
The technological side of colon cancer care is also evolving. Telemedicine and virtual consultations have expanded accessibility, particularly for people who live far from major medical centers or have mobility issues. Remote communication allows for regular check-ins about symptoms and treatment side effects, reducing the burden of frequent in-person appointments. These consultations also offer mental health support and educational resources through digital platforms. The growth in health-related mobile applications has introduced additional options for medication reminders, symptom tracking, and diet monitoring. However, these tools should be used in conjunction with—and not as a substitute for—professional medical advice.
In many communities, awareness campaigns and local events aim to break the stigma around colonoscopies and other screening procedures. These initiatives often focus on the importance of early detection and the relative simplicity of tests like the FIT, which can be done in the privacy of one’s home. Campaigns may also highlight success stories of individuals who detected their colon cancer early or even just discovered polyps that were removed before becoming malignant. Seeing these examples can encourage others to take proactive steps for their own health. For those who do not have insurance or worry about the financial cost, various programs and organizations provide support, from free screening events to financial assistance for medical bills. Accessibility is a major factor in improving outcomes across different populations.
Open, ongoing discussions with healthcare professionals form a cornerstone of colon cancer prevention and care. Patients who are well-informed about each step of diagnosis and treatment often experience less anxiety and a greater sense of control. Even the language used in medical settings is evolving to be more patient-friendly and less intimidating. When people feel comfortable discussing their symptoms and asking questions about procedures, they are more likely to follow through with screening recommendations and feel confident about treatment choices. Mutual trust and respect between patients and providers foster an environment where individuals can receive personalized care, adapted to their specific needs.
As research on colon cancer moves forward, scientists continue to study the role of various environmental toxins, gut microbiome imbalances, and cellular processes in driving or preventing cancer. One area that has garnered attention is the microbiome—the trillions of bacteria residing in our digestive tract—which influences everything from nutrient absorption to immune system regulation. Alterations in the microbiome could potentially pave the way for polyp formation and malignancies. While there is no one-size-fits-all solution to cultivating a healthy microbiome, diets rich in fiber, fermented foods (like yogurt and kefir), and limited in highly processed items are commonly recommended. Some experts are investigating whether probiotics or prebiotics might have a role in colon cancer prevention, though the research remains in early stages.
For individuals who are cancer-free but want to remain vigilant, routine follow-up appointments and screenings are essential. Healthcare providers may also suggest additional imaging or blood tests if there are any concerns about recurrence or if new symptoms arise. Maintaining healthy lifestyle habits after remission can be equally important, because the risk of recurrence persists for some time after successful treatment. By continuing to prioritize exercise, balanced eating, and stress management, survivors can bolster their overall health and reduce the likelihood of other chronic conditions. Psychologically, this sense of proactive engagement often offers a comforting feeling of control and optimism about the future.
Many different resources exist for those seeking information or community support related to colon cancer. Renowned institutions provide online educational materials, and nonprofit organizations frequently offer hotlines or patient navigators to help with questions about treatment, financial logistics, or finding local support groups. Social media has emerged as another forum where patients and survivors connect, although caution with online information is advised due to the spread of unverified sources. Reliable platforms advocate for evidence-based practices and direct people to peer-reviewed studies. By balancing professional medical advice, personal research, and community perspectives, individuals can feel more empowered throughout their entire healthcare journey.
Much progress has been made in demystifying colon cancer, but ongoing vigilance and education remain the linchpins of better outcomes. Having open discussions with family members can reveal important clues about possible genetic predispositions, and adopting consistent screening protocols can catch issues before they become advanced. A balanced, nutrient-dense diet, alongside regular exercise, supports overall health and helps counteract many of the lifestyle risks associated with colon cancer. The growth of targeted treatments and improved diagnostic tools offers renewed hope, enabling doctors to tailor therapies to each patient’s biological profile and thereby enhance effectiveness while potentially reducing side effects. Individuals have more tools than ever to maintain and improve their colon health, from preventive measures to advanced, personalized care plans. By staying informed and engaged, people can navigate the intricacies of colon cancer care with a sense of confidence and purpose, whether they are focused on prevention, undergoing active treatment, or supporting a loved one.
