Mental health is as vital as physical health, yet it remains shrouded in damaging myths that prevent millions from seeking help. These misconceptions fuel stigma, silence conversations, and even shape misguided policies. Let’s dismantle six pervasive myths with evidence, empathy, and clarity. Understanding the truth isn’t just about awareness—it’s about saving lives, strengthening communities, and fostering a society where no one suffers in shame. Imagine carrying a heavy backpack every day, but being told it’s “all in your head” when you ask for relief. That’s the weight of mental health stigma, and it’s time to set the record straight.
One of the most persistent falsehoods is the idea that mental health problems are rare. Nothing could be further from reality. Globally, one in four people will experience a mental health condition in their lifetime, according to the World Health Organization. In India alone, over 150 million people need care for mental health conditions—that’s larger than the population of Japan. Conditions like depression and anxiety aren’t niche issues; they’re as common as hypertension or diabetes. Consider the COVID-19 pandemic, which triggered a 25% surge in anxiety and depression worldwide. If mental health problems were rare, why do celebrities, athletes, and even historical figures like Abraham Lincoln openly describe their struggles? Prevalence doesn’t equate to visibility. Many suffer quietly due to fear of judgment, creating an illusion of rarity. Dr. Shekhar Saxena, former WHO mental health director, emphasizes, “Mental health conditions are universal. Ignoring them doesn’t make them disappear—it amplifies suffering.”
Another harmful myth claims that people with mental health conditions are violent or unpredictable. Media sensationalism fuels this stereotype—think horror films equating psychosis with danger. In truth, those with mental health issues are far more likely to be victims of violence than perpetrators. A landmark study in the British Journal of Psychiatry found they commit only 3–5% of violent acts, often linked to factors like substance abuse, not the illness itself. Contrast this with alcohol abuse, which is implicated in nearly 40% of violent crimes. Take Rahul, a Delhi-based engineer with bipolar disorder. When stable on medication, he’s a dedicated professional and father. His “unpredictable” label stems from one manic episode a decade ago—yet his colleague who drinks excessively faces no such judgment. Violence is a human issue, not a mental health one. Dr. Vikram Patel of Harvard Medical School states, “Fear of violence is a barrier to compassion. Most individuals with mental illness are just trying to navigate daily life, like anyone else.”
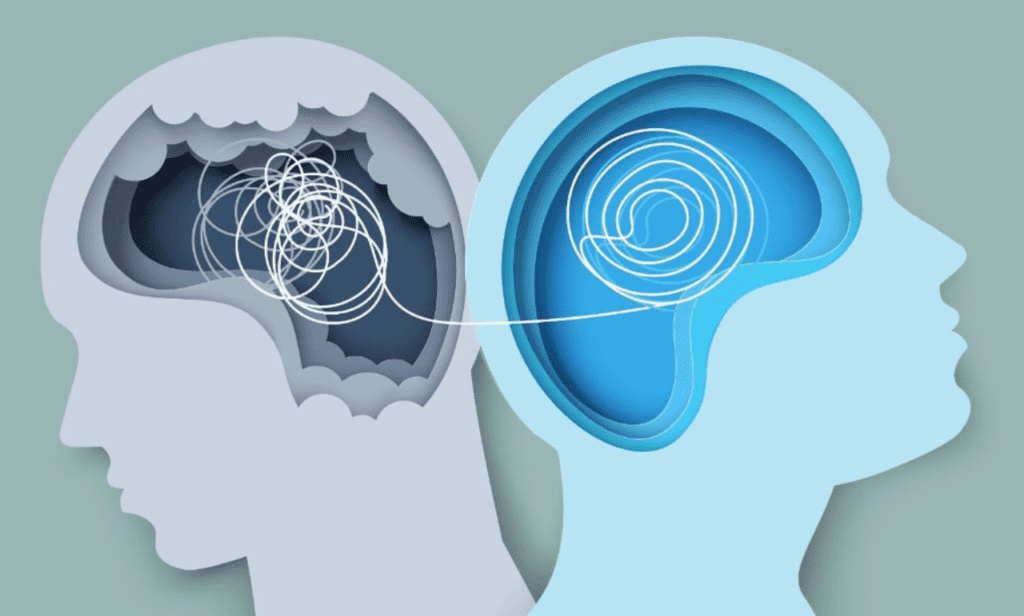
The myth that mental health struggles signal weakness is perhaps the most corrosive. It confuses biology with character. Mental health conditions arise from complex interactions between genetics, brain chemistry, trauma, and environment, not personal failure. Would we call someone “weak” for developing asthma or cancer? Depression, for instance, involves measurable changes in brain structures like the hippocampus, which regulates emotion. Research shows prolonged stress can shrink this region, making resilience physiologically harder. Consider Priya, a marathon runner diagnosed with depression. No one questioned her strength when she finished races, yet her aunt whispered, “Just pray harder,” when Priya started therapy. This bias ignores science: the American Psychological Association confirms mental health conditions require evidence-based interventions, not willpower. Cognitive Behavioral Therapy (CBT), for example, rewires neural pathways—a process demanding courage, not weakness. As author Johann Hari notes, “We’ve been told depression is a malfunction. What if it’s often a sane response to an insane world?”
The false choice between therapy and medication also needs debunking. Some insist pills are a “quick fix,” while others dismiss therapy as “talking nonsense.” Effective treatment is rarely one-size-fits-all. For severe depression, the combination of medication and therapy succeeds in 60–70% of cases, per the National Institute of Mental Health. Medication corrects chemical imbalances—like insulin for diabetes—while therapy builds coping tools. Conversely, mild anxiety might only require CBT. Ravi, a Kolkata teacher with OCD, found relief only after combining SSRIs with exposure therapy. Still, cultural barriers persist. India has less than one psychiatrist per 100,000 people, pushing many toward pills alone. But as Dr. Nimesh Desai, former director of IHBAS Delhi, explains, “Medication stabilizes, therapy empowers. Depriving patients of either is like offering a ladder with half the rungs missing.”
Another damaging assumption is that mental health conditions disqualify people from work or education. Performance hinges on support and management, not diagnosis. Stephen Hawking revolutionized physics with ALS. Kiran Mazumdar-Shaw built Biocon while managing anxiety. Studies reveal that employees with mental health conditions, when accommodated, show equal or higher productivity. Tech giant Infosys reports 92% retention rates for staff using their mental wellness programs. Flexible hours, remote options, or quiet spaces enable thriving—simple adjustments benefiting all. Conversely, untreated conditions cost the global economy $1 trillion yearly in lost productivity (WHO data). Schools, too, see success with interventions. A Mumbai college introduced exam breaks for anxious students; pass rates rose 15%. Mental health advocate Arun John argues, “Exclusion stems from myth, not evidence. With reasonable support, people contribute meaningfully.”
Finally, the myth that mental health conditions are lifelong sentences ignores recovery’s reality. While chronic cases exist (e.g., some forms of schizophrenia), many people recover fully or manage symptoms long-term. Eighty percent of depression patients improve within a year with treatment. PTSD recovery rates exceed 50% with trauma-focused therapy. Even severe conditions like bipolar disorder see 40–60% achieving significant stability. Recovery isn’t linear—relapses occur, like in diabetes—but they don’t define permanence. Sunita, diagnosed with panic disorder at 20, hasn’t had an attack in eight years through mindfulness and peer support. Modern approaches focus on “mental health journeys,” not cures. Dr. Brock Chisholm, the first WHO Director-General, declared, “Without mental health, there is no true physical health.” Embracing this fluidity reduces despair. As neuroscientist Dr. Tara Swart notes, “Neuroplasticity means our brains heal. Hope isn’t naive—it’s scientific.”
Dispelling these myths requires collective action. Share facts compassionately. Challenge jokes equating OCD with tidiness. Support workplace mental health policies. Most importantly, listen without judgment when someone shares their struggle. Every myth dismantled chips away at stigma, making it easier for a friend, parent, or colleague to seek help. Mental health isn’t a fringe issue—it’s the bedrock of human resilience. When we stop believing lies, we start building a world where healing isn’t hidden, but honored.
